
Like many broad legislative measures, Texas’ 2003 medical liability reforms continue to be a target for opponents long after being signed into law.
The Texas Medical Association is fighting again to defend them.
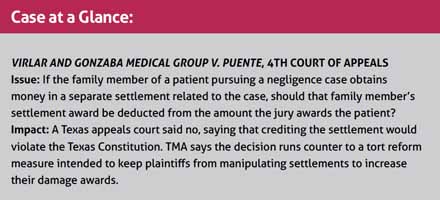
The measure under siege this time prevents patients who file negligence or other lawsuits from adding to their damage award through family members’ settlements stemming from the same case – that is, no “double-dipping.”
In a case that could land before the Texas Supreme Court, a physician ordered to pay about $14 million in a negligence suit is trying to reduce that award. He claims in court documents that a separate settlement between the plaintiff’s daughter and a hospital should be deducted from the $14 million.
TMA believes the law is on the side of Jesus Virlar, MD, and Gonzaba Medical Group (GMG) as they pursue that settlement credit. Thus far though, a Bexar County trial court and the 4th Court of Appeals have denied that effort. TMA will sign on to a brief with the Texas Alliance for Patient Access (TAPA) supporting Dr. Virlar and GMG when they ask the state’s high court to review the issue.
Edinburg gastroenterologist Carlos Cardenas, MD, remembers the pre-tort reform days to which no Texas physician wants to return. Among the many legal vulnerabilities doctors faced in those days, Dr. Cardenas recalls “an egregious use of the legal system to basically double-dip, [which] was then employed by the trial bar or others to try to find ways to increase … earnings [for] law firms.
“This judgment … flies in the face of the reforms that were voted on by the people of Texas,” he said, referring to Proposition 12, the referendum that helped usher in tort reform.
Giving proper credit?
According to court documents, Jo Ann Puente underwent gastric bypass surgery by Nilesh Patel, MD, in November 2011. She endured months of complications, during which Dr. Virlar, a hospitalist and employee of Gonzaba Medical, assumed her care at Metropolitan Methodist Hospital, court documents say. Metropolitan Methodist ultimately discharged Ms. Puente in early 2012, but she suffered permanent brain damage. Her treating neurologist testified she was later diagnosed with Korsakoff’s syndrome, an acute deficiency of thiamine, according to court documents.
Ms. Puente sued Dr. Virlar and Gonzaba Medical in March 2014, along with “numerous other health care providers” who were involved in treating her, including Dr. Patel and Metropolitan Methodist. She settled with everyone she sued except Dr. Virlar and GMG, which took their case to trial. A jury awarded Ms. Puente more than $14 million.
Separately, however, Ms. Puente’s minor daughter confidentially settled with the hospital over a “loss of consortium,” a claim often brought by family members if they believe an injury to their loved one deprives them of care and affection.
Dr. Virlar and Gonzaba Medical Group claimed that settlement amount should be deducted from the jury’s award in their case. As part of his argument, Dr. Virlar cited the section of the 2003 tort reform law that applies to settlement credits.
When a person, or “claimant,” seeks damages for injury to someone else, the law says the definition of “claimant” in that scenario includes both the person injured and “any person who is seeking, has sought, or could seek recovery of damages” for the injury, the law states. It also says that in certain cases, if the claimant has settled with one or more people while pursuing damages, the other side has the option of applying a settlement credit.
So Dr. Virlar argued Ms. Puente and her daughter, under the law, were one “claimant,” and Dr. Virlar and Gonzaba Medical Group are entitled to a credit to the damages the jury awarded.
“A claimant is everybody,” Diana Faust, an attorney for Dr. Virlar and Gonzaba Medical, told Texas Medicine. “In this particular case, it is Ms. Puente and all those who claim to have derivative claims based on her claim. She is the hub of the wheel, so to speak, and then the spokes, that’d be her daughter, her mother, whoever might have a right to … a derivative claim for loss of companionship, parent-child relationship, those types of derivative claims.”
Ms. Puente disagreed, saying Dr. Virlar was not entitled to that credit.
“The Supreme Court has made clear that a loss of consortium claim is a separate and independent claim distinct from the clams of the physically injured family member. It is quite clear under Texas law that a loss of consortium claim that a minor child has relating to a severe injury to a parent is a separate and independent cause of action,” Ms. Puente’s court documents state.
Attorneys for Ms. Puente did not return calls from Texas Medicine seeking comment.
Both a Bexar County district court and the 4th Court of Appeals disagreed with Dr. Virlar, declining to apply the settlement credit.
In its decision, the appeals court acknowledged that the law was “enacted as part of House Bill 4’s tort reform efforts to reduce costs to the health care industry. However … the Supreme Court has clearly stated that restricting economic damages awarded to victims of medical malpractice for the general goal of attempting to reduce overall costs to the health care industry” violates the Texas Constitution, Justice Liza A. Rodriguez wrote.
“Here, all the damages awarded by the jury to [Ms.] Puente are economic damages,” Justice Rodriguez added. “Thus, applying [the law’s] settlement credit provisions and reducing [Ms.] Puente’s award in an amount equal to [her daughter’s] settlement results in [Ms.] Puente recovering less than the full amount of her economic damages.”
TMA and TAPA spring into action
Ms. Faust says her clients plan to ask the state Supreme Court to review the settlement-credit issue, and TAPA and TMA plan to file a joint friend-of-the-court brief in support, stressing the importance of applying the settlement-credit law correctly.
“The settlement credit statute is certainly not unconstitutional. It just isn’t. It’s frustrating that the court went the direction that the court went,” said Brian Jackson, TAPA’s general counsel. He says when the Texas Legislature adopted tort reform, it wanted “to make sure plaintiffs didn’t get paid twice for their damages, even if they try to come up with some way to try and circumvent that.”
If the courts continue to allow the $14 million award to stand without the settlement credit, “it will increase exposure for all health care providers,” Mr. Jackson added. “Because plaintiffs will be allowed to double-dip and get paid for damages that they’ve already been compensated for, in my opinion. That increases exposure. That increases the insurance company’s evaluation of each case,” which could impact insurers’ ability to adequately cover physicians.
Dr. Cardenas has no interest in any reversion back to what Texas physicians were experiencing prior to 2003, when he and his colleagues felt “under siege.” TMA should continue to support the law as written, he says – and the legislature, not the bench, is the proper place to revisit it.
“Every [legislative] session, there’s a different tack taken by the plaintiffs’ bar and those representing plaintiffs to try to undo what we did,” Dr. Cardenas said. “It’s an ongoing struggle, and we need to remain vigilant.”
Tex Med. 2020;116(5):25-27
May 2020 Texas Medicine Contents
Texas Medicine Main Page
Tex Med. 2020;116(5):25-27
May 2020 Texas Medicine Contents
Texas Medicine Main Page