Like many physicians, Cedar Park internist Manish Naik, MD, started using Direct Secure Messaging (DSM) to comply with requirements levied by the Centers for Medicare & Medicaid Services (CMS).
“Initially, it was more about checking a box than making it a meaningful use of data exchange,” he said.
That was five years ago. Since then, the technology has grown more popular – and meaningful.
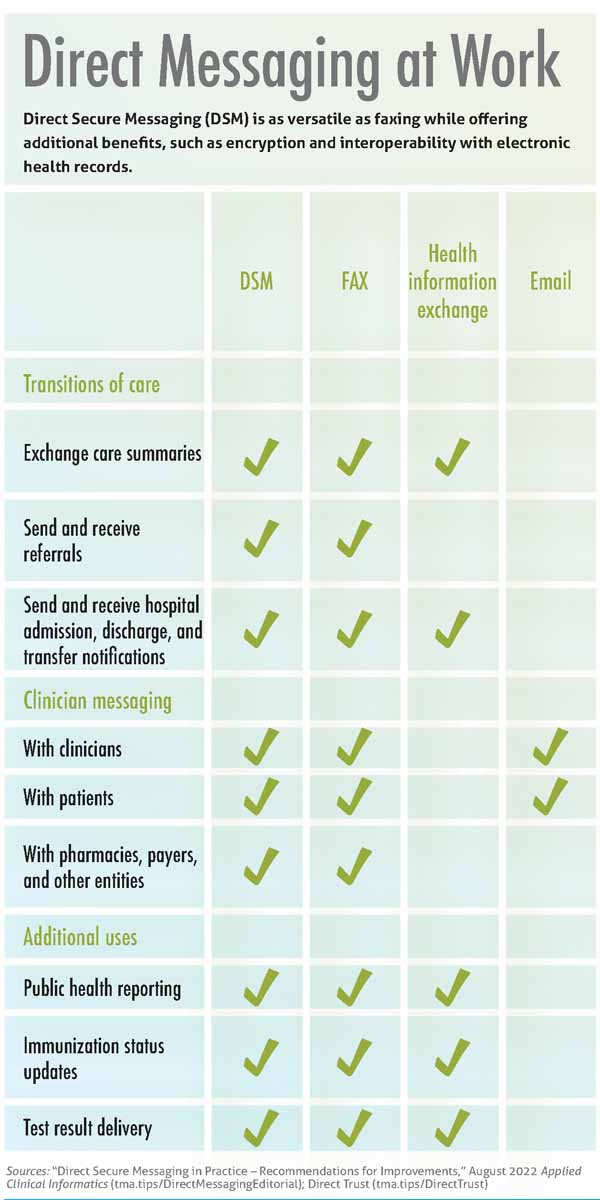
DSM, or Direct messaging, is a low-cost, electronic communication method similar to email that allows physicians to exchange protected health information over the internet in a secure, HIPAA-compliant manner. (See “Direct Messaging at Work,” page 22.)
Yet, unlike email or a health information exchange (HIE), Direct messaging is as versatile as faxing and can be used to send and receive referrals as well as to communicate with pharmacies, payers, and other entities. It also offers increased security when compared with fax machines – which can be hacked, intercepted, or busy – and improves interoperability across electronic health record (EHR) vendors, which is a persistent thorn in physicians’ sides.
Federal policies have helped drive adoption, and experts say practices that use Direct messaging enjoy these benefits as well as freedom from manual data entry drudgery.
By the end of 2021, there were nearly 2.8 million Direct addresses in the U.S., up 12% year over year and more than four-fold since 2014, according to DirectTrust, a nonprofit trade alliance and standards body that accredits Direct messaging providers.
But Dr. Naik, chief medical information officer at Austin Regional Clinic (ARC) and a member of the Texas Medical Association’s Committee on Health Information Technology, cautions there are some kinks to smooth out before Direct messaging lives up to its potential.
He worked with ARC’s staff, its EHR vendor, and area hospitals to troubleshoot Direct messaging challenges, attendant with any new technology. Thanks to this investment, ARC physicians and support staff have made progress, and they’re more consistently getting information from hospitals, reducing the need to request faxed records.
For instance, if one of Dr. Naik’s patients visits an emergency department, he can review any notes from that visit via Direct message during the follow-up appointment at ARC and then upload relevant information directly into his EHR for future reference. Similarly, primary care physicians use Direct messaging to access patient notes from specialists – regardless of their EHR vendor – and incorporate them into their own EHR.
“We’re making very significant progress. We’re getting more of the data [we need] more consistently,” he said. “The challenge, in my mind, is that every health care [professional], health care group, and health care system shouldn’t have to go through this [troubleshooting] process. There ought to be standards for how the EHR is set up to receive information” via Direct message.
Dr. Naik would like to see EHR vendors improve their Direct messaging services so that other groups – especially solo, small, and rural practices with limited resources and no IT department – can reap the same benefits.
Fortunately, the Texas Health Services Authority (THSA), a public-private partnership whose board includes physicians, has convened a work group to take on this task. Its member organizations, including TMA, aim to improve Direct messaging so that every practice willingly opts in – and can put the kibosh on faxing once and for all.
Demystifying DSM
The Health Information Technology for Economic and Clinical Health Act of 2009, known as HITECH, promoted “meaningful” use of health information technology and in so doing helped initiate the development of Direct messaging in 2011. Five years later, CMS required EHR vendors to provide Direct messaging services. Two public HIEs in Texas – Greater Houston HealthConnect and Healthcare Access San Antonio, or HASA – also offer Direct messaging.
Now the technology factors into compliance with more recent regulations. That includes a 2020 federal requirement for physicians to update their digital contact information, such as a Direct address, in the National Plan and Provider Enumeration System, as well as the 21st Century Cures Act’s information-blocking rules, which took effect in April 2021. (See “Information Unblocked,” June 2022 Texas Medicine.)
Fort Worth family physician Craig Kneten, MD, is a Direct messaging evangelist, citing its ease of use and patient benefits.
“It’s basically just email, and it’s HIPAA-compliant,” he said. “I love this idea.”
Dr. Kneten, who serves on the THSA work group, predominantly uses Direct messaging to communicate with large health systems. Since May 2021, CMS has required hospitals to send admission, discharge, and transfer notifications electronically, such as by using Direct messaging.
Direct messages can take different forms, such as PDFs or images. Depending on the format, message elements may be incorporated by the receiving EHR, improving interoperability across vendors.
When hospital notifications arrive via Direct message, Dr. Kneten says he can review them in “just a couple of clicks,” before forwarding them to his medical assistant, with a request to schedule a follow-up appointment.
This interoperability “saves an awful lot of time” when compared with electronic faxing, he said.
Although his practice uses artificial intelligence to parse electronic faxes and transfer the relevant information to his EHR, Dr, Kneten says such software isn’t a perfect solution. As a result, his staff still spends a lot of time scanning electronic faxes – which are not searchable - into his EHR. Dr. Kneten also uses Direct messaging to access patient notes from specialists, which automatically populate his EHR, no scanning required. In both applications, Direct messaging helps to facilitate follow-up care and minimize physicians’ administrative burden.
Still, he acknowledges Direct messaging can seem opaque to those who aren’t already familiar with it.
For starters, the service is often relegated to the background, one of many administrative tasks that physicians must complete each day, according to an August 2022 editorial published in Applied Clinical Informatics.
“Most clinicians are familiar with EHR-based electronic communication within a health system, and some may be aware of electronic communication across organizations that use the same EHR vendor,” the authors wrote. “However, fewer are aware of [Direct messaging], which facilitates EHR-based electronic communication by health care organizations using different EHR systems … even if they use it daily.”
EHR vendors also use different names for Direct messaging – Care Everywhere, Direct, Direct Email, DSM, eClinical Direct, eReferral, and NextGen Share, among others – which can cause confusion among users, according to the editorial.
TMA experts say these issues belie Direct messaging’s utility, especially when compared with faxes, which remain a common means of sharing protected health information despite widespread adoption of EHRs.
A 2019 Medical Group Management Association poll found 89% of health care leaders reported their organizations still use fax machines. This is the same share of Texas physicians who said their organizations had implemented an EHR, according to a 2020 TMA survey.
Dr. Kneten worries faxes contribute to patient harms, such as if a paper message containing imaging results or notice of a hospital admission is lost on its way to him, delaying much-needed treatment or interfering with continuity of care.
“I really think using fax technology from the last century is a risk to patients,” he said.
Katherine Lusk, vice president of strategic partnerships at THSA and a co-author of the aforementioned editorial, says Direct messaging resolves these security concerns by requiring identify verification. And clinicians can only receive Direct messages from a sender who is known to them, cutting down on the possibility of spam.
She adds that Direct messaging also may offer time savings.
A recent THSA review of one EHR vendor found it took four steps to upload information from a Direct message into the EHR, compared with 17 steps to upload the same information from a fax.
Although Direct messaging services vary across EHR vendors and HIEs, they can help physicians maximize their time with patients and minimize their time spent on EHRs, which is considerable. A 2020 study in the Annals of Internal Medicine found physicians spend more than 16 minutes, on average, per patient encounter using EHRs.
Lessons from early adopters
Despite Direct messaging’s benefits, the service poses some unresolved challenges, which have hindered universal adoption.
Dr. Naik says his early experience with the service at ARC was “very hit or miss,” citing inconsistent message formatting and increased clinician administrative burden as concerns.
There are other issues, according to Applied Clinical Informatics. For instance, there is no universal Direct address directory. Instead, most EHR vendors compile one for their own users, but these are limited and provide little help to physicians searching for an addressee who uses a different vendor.
Similarly, not all practices have transitioned to an EHR. Among those that have made the switch, some have yet to adopt Direct messaging, even if their EHR vendor offers the service free of charge. Until Direct messaging is the standard, practices that use the service likely will continue to rely on faxes and other kinds of messaging, which may interrupt their workflow.
The influx of Direct messages also may overwhelm practices. Hospital admission, discharge, and transfer notifications – sent electronically as required by CMS – quickly pile up in physicians’ inboxes, adding to their administrative burden and cutting into time with patients.
Dr. Naik says these notifications initially proved frustrating for ARC. Sometimes, they weren’t of clinical value, such as a message indicating a patient had signed into a hospital’s front desk. Other times, their formatting meant they weren’t compatible with ARC’s EHR. As a result, a service that was meant to save physician and staff time required more of it.
“It took a lot of troubleshooting with our organization, the hospital technical folks, and with our electronic health record vendor … to finally figure out where those setting adjustments were,” he said.
These headaches – and the work required to resolve them – can dissuade practices from adopting Direct messaging, exacerbating the patchwork quality of health care communications and inuring practices to less secure modes of communications.