
Texas Gov. Greg Abbott in February listed the fentanyl crisis as one of seven “emergency” items this session, clearing a path toward passage of Texas Medical Association-backed legislation that aims to curb opioid-related deaths.
Illicitly produced fentanyl causes most opioid overdoses in the U.S., including in Texas. In 2018, Texas saw 210 deaths associated with fentanyl, but that rose to 1,612 by 2021, according to the Department of State Health Services. In 2021, fentanyl was tied to 95% of all unintentional synthetic opioid deaths in the state, the agency says.
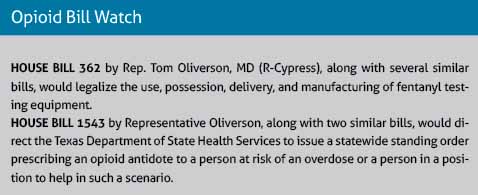
TMA is tracking several measures that could help improve the state’s crisis response by legalizing fentanyl test strips, increasing the state’s supply of the opioid antidote naloxone, and easing physician use of Texas’ prescription monitoring program (PMP). (See “Opioid Bill Watch,” right.)
Governor Abbott signaled his support for these bills during his Feb. 16 State of the State address, saying Texas must “increase the supply of lifesaving Narcan” – a brand name for naloxone – “so we can save more Texans who are ambushed by fentanyl.”
The bills could be fast-tracked given Governor Abbott’s declaration of the fentanyl crisis as an emergency item this session.
Meanwhile, developments at the federal level also are paving the way toward solutions by increasing access to opioid disorder treatments and overdose-reversing drugs.
In addition, Texas’ preliminary budget bills from both the House and the Senate include funding for licensing fees related to the PMP, which physicians are required by state law to consult when prescribing certain opioids and other controlled substances.
Physicians don’t have to pay to access the PMP, but they do have to pay fees to keep their electronic health record integrated with the program. Michelle Romero, TMA associate vice president of public affairs, says the $7 million budget item could help remove what has amounted to an “unfunded mandate” for physicians over the past few years.
Testifying on TMA’s behalf, Mesquite pain management specialist C.M. Schade, MD, endorsed these interventions, along with other TMA recommendations, during a Sept. 13 interim meeting of the House Committee on Public Health. He is a member of TMA’s Subcommittee on Behavioral Health.
“The ‘opioid crisis’ is no longer just about prescription opioids,” he testified, emphasizing that the main driver is illegally manufactured fentanyl. “It is time for us to reexamine our processes and change course.”
TMA’s other recommendations include:
- Investing in effective data mining software to compare pharmacy purchases with pharmacy PMP sales to spot illegal prescribing and dispensing;
- Improving education and prevention programs about opioids;
- Expanding mental health and substance use disorder services;
- Improving data collection to identify at-risk populations; and
- Creating community-based syringe service programs, which can connect people with addiction to the larger health care system for treatment and other services.
Federal progress
Recent federal efforts also could give states a boost in the fight.
The U.S. government recently ended a major restriction on prescribing buprenorphine, one of the most effective medications for treating opioid use disorder.
Passage of the Consolidated Appropriations Act of 2023 swept away the need for an “X waiver” for physicians or other health care professionals to be able to prescribe buprenorphine, according to the Drug Enforcement Administration (DEA).
Since 2000, physicians have been required to obtain an X waiver under the Drug Addiction Treatment Act. Among other things, the waiver required physicians to take an eight-hour training program before being able to prescribe buprenorphine. Other health care professionals had to take 24 hours of training.
“On top of that, it gave the DEA authority to visit physician practices unannounced to specifically audit buprenorphine prescribing,” said Carlos Tirado, MD, an Austin addiction psychiatrist and member of TMA’s Subcommittee on Behavioral Health. “It created an adversarial environment in which physicians experiencing these DEA on-site practice audits often felt that they were being treated like criminals for treating a chronic medical condition.”
A 2021 rule change by the U.S. Department of Health and Human Services allowed physicians to opt out of the eight-hour training – though they still had to obtain the waiver and face audits. Also, those who opted out could treat only 30 patients with buprenorphine for opioid use disorder.
The Consolidated Appropriations Act eliminates X waivers entirely, including special audits or restrictions on the number of patients, according to the Substance Abuse and Mental Health Services Administration (SAMHSA).
“All practitioners who have a current DEA registration that includes Schedule III authority, may now prescribe buprenorphine for opioid use disorder in their practice if permitted by applicable state law and SAMHSA encourages them to do so,” the agency said.
Complex cases of opioid addiction – like those with underlying problems with mental health or infectious disease – will still require input from addiction specialists, Dr. Tirado says. But eliminating the X waiver will make it easier for primary care physicians to initiate care or maintain care for patients who are stable on the medication.
“Restricting buprenorphine during the worst opioid crisis of our lifetimes probably contributed to making the opioid epidemic worse,” he said.
Similarly, as of press time in early March, two panels of medical experts had unanimously recommended to the Food and Drug Administration (FDA) that Narcan nasal spray, which can reverse an opioid overdose, be made available over the counter – a move Texas physicians have long championed. A final FDA decision was still pending.
The goal of the FDA panels’ recommendation is to make the naloxone spray cheaper and more widely available so that more people can prevent opioid overdoses, Dr. Schade says.
An opioid overdose slows respiration until a person stops breathing, he says.
“After that, you have about five minutes before you’re brain dead,” Dr. Schade said. “What that means is that you have to have [Narcan] rapidly available.”
Pharmacies in most states – including Texas – are allowed to use a standing order from a physician to provide the medication to anyone who wants to buy it. But people still must pay whatever copay their insurance requires, and that can drive up the price, he adds.
Making Narcan available over the counter should lower the cost for consumers and make the medication as common as other over-the-counter medications.
“If it’s over the counter, the price will go down, and people will have it,” he said. “Through education, it will be widely available in first-aid kits and be omnipresent.”
Narcan nasal spray poses no safety risk for the public, even for children, adds Dr. Tirado.
“Naloxone is incredibly safe,” he said. “In fact, it’s one of the safest medications out there. There’s really no reason this shouldn’t be over the counter.”
The recommendation for Narcan’s over-the-counter use came from a joint meeting of the Nonprescription Drugs Advisory Committee and the Anesthetic and Analgesic Drug Products Advisory Committee. The unanimous vote by the committees’ 19 members was nonbinding, but FDA typically follows recommendations by its expert medical panels.