
Abilene family physician Zoie Walker, MD, recalls the struggle her grandfather faced after being diagnosed with multiple sclerosis.
At the time, their hometown of Cross Plains had a population of fewer than 1,000 residents and even fewer doctors, forcing her grandfather to drive miles to receive necessary medical care.
“My grandfather’s condition inspired me to pursue a career in medicine,” she said. “One of my goals as a physician is to provide care to those who go without, and I know firsthand that that includes rural patients.”
According to Rural Health Information Hub, more than 3 million Texans live in rural designations, and, per the U.S. Department of Health and Human Services (HHS), 119 of the 172 rural counties in Texas are identified as primary care health professional shortage areas.
Dr. Walker knew she wanted to treat rural patients like her grandfather but needed help.
“My parents are not physicians,” she said. “But that doesn’t mean I wasn’t introduced to medicine at a young age. I wanted to learn more about medicine, so I reached out to a group that offered resources and information to kids like me with questions about a career in health care – and that group was our local county medical society alliance.”
Abilene’s local alliance chapter, the Big Country County Medical Society Alliance (BCCMS Alliance), provided community support and scholarship funds that Dr. Walker used while she attended medical school at Texas Tech Health Sciences Center School of Medicine (TTUHSC) in Lubbock. She also did her residency there.
Sue Schackmuth, a past president for the BCCMS Alliance, says the scholarship was created to help medical students without a familial background in health care, like Dr. Walker. The funds, raised by BCCMS Alliance members and donations from the Anson Jones Memorial Medical Foundation, among other sources, have supported many of Abilene’s physicians.
Dr. Walker says the scholarship encouraged her to practice in Abilene, where she now treats a patient population that includes rural residents from surrounding counties.
“I received a scholarship from the alliance that enabled me to achieve my goal of becoming a physician,” she said. “It made the choice to practice in Abilene, near my hometown, an easy one.”
Hometown connections
Although Abilene is not a physician shortage area, its surrounding areas are. For example, adjoining counties like Nolan, Jones, and Callahan counties rank 80th, 172nd, and 213th, respectively, in terms of physicians per 100,000 people out of 254 counties, according to the Texas Department of State Health Services (DSHS).
Many of those residents drive to Abilene for treatment, says Ms. Schackmuth. “And we have a reach to provide care for many more.”
Physicians who understand rural health care needs and return to the area to practice make a “substantial difference for the community,” says internist and fellow BCCMS Alliance scholarship recipient Austin Lunney, MD.
According to DSHS, current projections for medical education enrollment indicate that Texas’ medical education system will not create a supply of physicians that will meet future demand.
However, Texas ranks second in the country in the retention of medical school graduates for practice (61.3%), per the American Association of Medical Colleges. DSHS reports that more than half (58.9%) of physicians who complete their graduate medical education (GME) in Texas stay in the state to practice after residency – knowledge that compelled the BCCMS Alliance to provide over $100,000 to allied health and medical school students for more than 30 years, says Ms. Schackmuth.
Dr. Lunney, who used the funds for test preparation materials for his medical licensure exam, credits the assistance with his return to Abilene and a “reconnection” to his community. The TTUHSC graduate also spent time away during residency at the Texas A&M Health Science Center in Bryan.
Recalling the connections he made with the alliance’s help, Dr. Lunney decided to move back to his hometown with his family and begin construction on a new home.
“I grew up in Abilene but wasn’t sure if I’d practice medicine there,” he said. “But when the alliance offered my scholarship, it alleviated the financial stress of medical school and opened the door to returning to my community. Scholarship opportunities like these are what keep Texas medical students in the area.”
Alliance scholarships are just one step towards creating a healthier Texas physician workforce. In 2023, TMA again built on years-long efforts to gain additional state support to produce and retain more physicians in the state to help alleviate the shortage.
Wins include increased funding for GME, physician residency programs, medical school tuition loan repayment, telemedicine expansion, and broadband access.
Notably, state lawmakers budgeted $233 million in the 2024-25 biennium – up 17% compared with the 2022-23 biennium – for the GME Expansion Grant Program, which supports the creation of new residency slots necessary to maintain the target 1.1-1 ratio of slots to medical school graduates. The legislature also allocated $116 million – up 12% – to residency training programs sponsored by medical schools; this funding helps offset the cost of teaching residents.
Other winners were:
- The Family Practice Residency Program, which will receive $16.5 million in 2024-25, up from $9 million in 2022-23. Its grants go to the state’s nationally accredited family medicine residency programs to increase the number of physicians who choose that specialty.
- Residency programs sponsored by Texas medical schools, which will receive a $12.6 million increase to support faculty costs and keep up with the recent growth in the number of residents.
- The Rural Residency Training Program, which will receive an inaugural allotment of $3 million. TMA initiated the 2019 creation of this program, which will issue grants to fund new residency positions in nonmetropolitan areas.
- The Physician Education Loan Repayment Program, which will receive $35.5 million, up from $29.5 million. The program incentivizes primary care physicians and psychiatrists to practice in rural and underserved areas by paying off their student loans.
- The Primary Care Preceptorship Program, which will receive a $2 million boost to promote an interest in primary care careers among medical students.
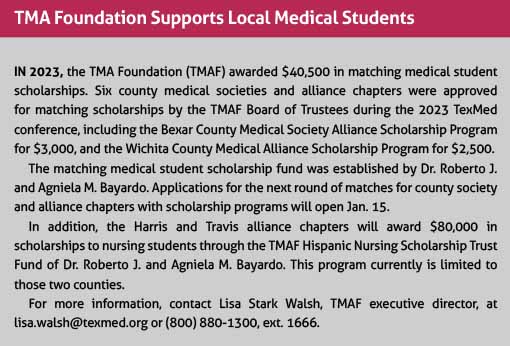
Additionally, the TMA Foundation’s Family of Funds awards matching medical student scholarships to county societies or alliance chapters that have their own medical student scholarship program. (See “TMA Foundation Supports Local Medical Students,” below.)
Medical students can apply for the BCCMS Alliance scholarship every year they are in medical school. Applications are open until April 1, with information found on the Community Foundation of Abilene website.
Dr. Lunney, who was introduced to the alliance as he grew up alongside Ms. Schackmuth’s children in school, believes the organization enabled him to practice in Abilene. Without its support, he says, he may not have returned to the area – or been introduced to medicine at all.
“I didn’t have family members in medicine, so I didn’t have access to a lot of information,” he said. “But through personal connections with the alliance, I was exposed to medicine and the resources I needed to become a physician. And that’s how you fight a physician staffing crisis – through hometown connections.”