
A successful emergency medicine residency program. A positive Match Day track record. And a community in need of care.
“I never in a million years thought that this would ever happen,” said Craig Pedersen, DO, an emergency medicine physician at CHRISTUS Spohn Hospital in Corpus Christi and director of academic progression for the residency program.
“This” was an unexpected announcement by CHRISTUS Spohn Hospital on Oct. 12 that it planned to close the training program based on “available resources” – a move that shocked the medical community.
And the foreseeable outcome was unacceptable to it.
“This [closure] would have been crippling to the community’s [emergency department] care for decades,” Dr. Pedersen told Texas Medicine.
The program faculty and residents quickly mobilized, reaching out to local leaders and testifying before local government entities.
Dr. Pedersen and his colleagues coordinated a grassroots advocacy effort that spanned Corpus Christi City Council, the Nueces County Commissioners Court, and the Nueces County Hospital District.
Thanks to their care and funding from the hospital district, CHRISTUS Spohn Hospital reversed its plan to shutter the CHRISTUS Health-Texas A&M Spohn Hospital Emergency Medicine Residency program in 2026.
As important, the faculty and residents developed a playbook for their peers facing similar residency program closure announcements, says Gary Floyd, MD, a retired pediatrician who lives in Corpus Christi and immediate past president of the Texas Medical Association. (He also is Dr. Pedersen’s father-in-law.)
“We have a blueprint here of how TMA and county medical societies can work with the existing faculty to help muster community support to maintain their programs,” he said. Especially given the physician workforce shortage in Texas, “we need more residency training programs [in Texas].”
The white coat treatment
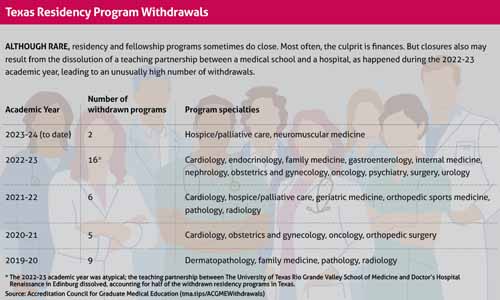
The Accreditation Council for Graduate Medical Education reports the withdrawal of 21 accredited U.S. residency programs so far during the 2023-24 academic year, including The University of Texas Rio Grande Valley School of Medicine’s hospice and palliative medicine program (effective September 2023) and UT Health San Antonio Long School of Medicine’s neurology residency program (effective June 2024). Residency program openings outpaced closures, however, with 118 new programs reported over the same period, including 17 in Texas. (See “Texas Residency Program Withdrawals,” below.)
Dr. Pedersen says the faculty banded together and spoke publicly, allowing program leadership to work with hospital administrators toward a lasting solution and allowing residents to focus on their training and clinical responsibilities. They earned the community’s support by showing up to public meetings en masse and explaining the stakes of closing an emergency medicine residency program in an underserved region.
“It was a pretty impactful visual,” Dr. Pedersen said of the group’s white-coat attire.
The Nueces County Medical Society (CMS) and TMA also got involved, echoing the pleas of program faculty.
In an Oct. 20, 2023, op-ed published in the Corpus Christi Caller Times, Nueces CMS President Reuben Pedraza, MD, and TMA President Rick Snyder, MD, urged CHRISTUS Spohn Hospital to reconsider and called on local leaders, including at the Nueces County Hospital District, to provide greater oversight of residency programs.
“Many residents in our community are indigent or have limited resources, so emergency services are the only way to access needed health care,” they wrote. “We feel it is crucial to continue to train emergency department physicians locally to help fulfill those needs.”
Thanks to the physicians’ campaign, CHRISTUS Spohn Hospital and the Nueces County Hospital District reached an agreement in early December to continue the residency program for at least six more years, through 2029.
“With this enhanced partnership with the hospital district, we will be able to confidently invite more classes of residents into the program in the future knowing they will have a sustainable and high-quality learning experience at CHRISTUS Health,” the hospital said in a statement shared with Texas Medicine.
Kelly Sandall, DO, a second-year resident in the program, looks forward to mentoring the incoming class of residents, which he sees as a key element of his training, and to continuing caring for underserved patients.
“Now that the residency is guaranteed [through 2029], it’s so nice to tell people confidently, ‘We’re here to stay,’” he said.
Planning for the future
Program faculty express hope this deal will serve as a stopgap until a long-term solution is found. They also are grateful for their community, local elected officials, and organized medicine for supporting their cause.
“It was incredibly heartwarming and really special seeing people of whatever political persuasion coming together for a cause like this,” said Michael Brodeur, MD, an emergency medicine physician at the hospital and curriculum director of the residency program.
Dr. Pedersen says the experience was a galvanizing one.
“It’s underscored the importance of being willing and able to advocate for yourself and your colleagues and your impact,” he said.
Texas’ physician workforce shortage is especially acute in rural areas, which struggle to recruit physicians, Dr. Floyd adds, commending the faculty and residents for ensuring the program’s survival.
“Their best pipeline is a local training program.”