
Dallas cardiologist Rick Snyder, MD, is a 37-year member and immediate past president of the Texas Medical Association. But he only recently joined the American Medical Association.
Spurred by his TMA presidency and the state medical association leadership’s involvement in the national organization, Dr. Snyder paid his inaugural AMA membership dues in early 2023. He even represented two specialty societies in the AMA House of Delegates during its annual policymaking session later that year.
“I went from nonmember to member to alternate delegate and then delegate within three months,” he told Texas Medicine.
During that time, Dr. Snyder reconsidered his reservations about AMA, including that it focuses too many of its resources on social matters rather than on “the bread-and-butter issues that affect all physicians,” such as practice viability and physician autonomy.
He also witnessed “the enormous respect and huge deference” paid to the Texas Delegation to the AMA and to TMA, both of which have led on these issues, including Medicare physician payment reform, prior authorization reform, and ensuring the fair implementation of the federal No Surprises Act.
“I see the value now,” he said.
Dr. Snyder hopes other Texas physicians will undergo a similar conversion.
The Texas Delegation’s success belies its relatively small size. This is largely due to strategy; the delegation is an aggressive coalition builder and campaigner for positions on AMA’s board, councils, and committees.
But David Henkes, MD, a pathologist in San Antonio and chair of the delegation, believes the group could be even more successful at full strength, and he encourages TMA member physicians to join AMA if they haven’t already.
“TMA membership is only half the job since at least half of our issues are federally involved,” he said, adding that TMA’s membership in AMA is at 34% with significant room to grow.
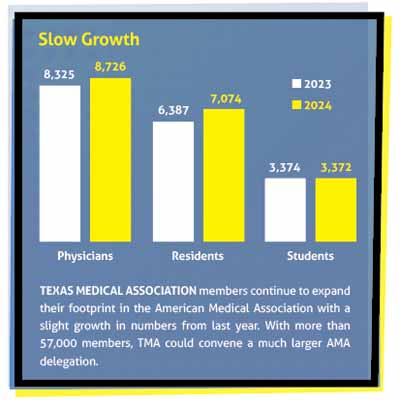
Between 2023 and 2024, Texas membership in the AMA grew 6%. To build on this momentum, the TMA House of Delegates recently adopted policy at TexMed focused on increasing AMA membership, especially among TMA leaders. Ironically, the reasons some Texas physicians have for not joining AMA, including diverging policy goals and the cost of dues, double as incentives.
“Like it or not, AMA is our representative,” Dr. Henkes said. “We need to get in there ... and guide the AMA to be more effective.”
As this story went to press, the TMA House also had directed the delegation to take nearly a dozen resolutions to the AMA House in June. Resolution topics focus on practical issues, including problematic health plan policies that impinge on physician payments and artificial intelligence’s (AI’s) health care applications.
Michelle Berger, MD, an ophthalmologist in Austin and a vice chair of the Texas delegation, also cites AMA’s recent success reducing the 2024 Medicare physician pay cut from 3.4% to 1.7%, which she attributes to its sway with Congress.
Thanks largely to the Texas delegation, AMA has prioritized comprehensive Medicare physician payment reform to ensure future Medicare physician fee schedules are not only cut-free but also keep pace with inflation.
“It does look like a lot of money when you have to write a check for [AMA] dues,” Dr. Berger said. “But ... if we can save you a 1% cut in your fees, we’ve already [covered] your membership.”
Full strength
TMA wields its influence on AMA in two ways: through the Texas Delegation and through membership on AMA’s various council and committees.
The AMA bases its state delegate count on association membership, with roughly one delegate apportioned for every 1,000 members. TMA is the largest state medical association in the country, with more than 57,000 members, but only about a third as many Texas physicians belong to AMA. This translates to a 20-person delegation, the third largest in the AMA House behind California’s and New York’s.
“If we could get everyone to become a member of AMA, we’d get 57 votes,” said Gary Floyd, MD, TMA past president and vice chair of the Texas delegation. “It’s [a] simple law of numbers.”
The delegation also maximizes “representation per delegate” by partnering with other states to achieve common goals and by recruiting members who meet AMA’s current and future needs, Dr. Berger added.
For instance, the Texas delegation is a member of the Big Four Coalition – along with the Florida, California, and New York contingents – as well as a founding member of the Key Issues Coalition, both of which wield their size in service of preserving the sanctity of the patient-physician relationship.
“We want to minimize the divisiveness and maximize our working together and effectiveness,” Dr. Henkes said.
The Texas Delegation builds relationships in other ways, too. Before the COVID-19 pandemic, Dr. Berger – along with Linda Villarreal, MD, and Diana Fite, MD, both TMA past presidents and current delegates – would post photos on social media from AMA meetings to demystify the process and encourage their followers in medicine to join. The posts became so popular that other delegates would photobomb the “Three Musketeers,” as they had become known.
“The social side of it is just as important,” Dr. Berger said. “You can’t pass policy if you don’t have social skills.”
Over the past decade, the Texas Delegation also has developed a pipeline of members whose skill sets – for example, graduate medical education in rural areas – make them strong contenders for AMA’s governing bodies, like its Council on Medical Education.
“The current amazing thing, which has never happened in the history of the delegation, is we have a [TMA] member on every single [AMA] council and committee except for [the Council on] Constitution and Bylaws,” Dr. Berger said.
As of this writing, Zeke Silva, MD, a radiologist in San Antonio and an alternate delegate, was one of four candidates running for three open seats on AMA’s Council on Medical Service, which serves a similar function as TMA’s Council on Socioeconomics. As chair of the AMA’s Specialty Society Relative Value Scale Update Committee, he oversees a volunteer group of 32 physicians and other health care professions who advise Medicare on how to value a physician’s work. He feels this role has been good training for the council.
“It’s really influential, and, for me, it’s what I love to do,” he said.
Dr. Silva also values AMA’s role as a solver of the payment problems facing physicians at the grassroots level. Sometimes, the national association draws on state-level wins, such as Texas’ 2021 “gold card” law, which hinged on TMA advocacy and has inspired similar prior authorization reform legislation in Congress. Other times, AMA facilitates inter-state collaboration, arming delegates with information that could help their peers back home.
“It’s very much bidirectional: local to national, national to local,” he said of AMA’s policymaking process.
Also at press time, Melissa Garretson, MD, an emergency physician in Fort Worth, was running with TMA’s endorsement for one of four open AMA board seats against six other candidates. John Carlo, MD, a public health specialist in Dallas and TMA board member, plans to run for an AMA board seat in 2025.
Read Texas Medicine Today for AMA election results.
Policy goals
Dr. Floyd, a retired pediatrician in Corpus Christi, is familiar with the AMA policy making process and how TMA exerts its influence.
An AMA member since 1976, Dr. Floyd joined the Texas Delegation in 2006. He chairs the AMA Council on Legislation.
“One of the goals all along for our delegation ... has been trying to make issues relevant to Texas, to TMA, also relevant to AMA,” he told Texas Medicine.
These issues often center on reducing administrative red tape and were reflected in the 11 resolutions that the delegation had planned to take to the AMA House, which, at press time, was slated to meet on June 7-12 in Chicago. House business can be found on the national association’s website (tma.tips/AMAHouse).
Several resolutions focus on health plans’ physician payment policies. At the direction of the TMA House, the delegation will introduce policy that would require AMA to advocate for federal legislation:
- Requiring plans to accept electronic submission of medical records, thus freeing medical practices from having to fax or mail them; and
- Preventing plans from automatically denying or downcoding claims, a practice that has repercussions on physician practice viability and patient access to care.
The TMA House also prioritized existential issues, such as erecting safeguards around AI. Specifically, the Texas delegation will propose amendments to AMA’s existing augmented intelligence policy, reiterating that any use of AI in patient care should be augmented by physician decision-making.
Dr. Henkes underscores the importance of such collective policy maintenance in the face of fast-moving technological advancements.

“We need to be sure and get this right and not get behind the curve on this ... so we can be sure patients are treated appropriately,” he said.