
When the Centers for Medicare & Medicaid Services (CMS) in July proposed a fifth consecutive round of cuts to physicians’ Medicare payments – contributing to a nearly 30% lag behind inflation growth since 2001 – medicine immediately mobilized.
“There’s no other business model that works where you decrease your amount that you pay a person every year,” said Gary Sheppard, MD, TMA chair of the Texas Medical Association’s Council on Socioeconomics. “We’re hoping [lawmakers] will realize that that’s not a sustainable way for physicians to be in practice and for patients to have access to physicians.”
TMA took action through an American Medical Association work group to forge a four-point reform proposal, the centerpiece of which is inflationary updates to physician payments via House Resolution 2474, along with:
- Updates that allow for more accurate estimates of physician payment versus being tied to “budget neutrality” constraints that require any payment increases or decreases to be offset;
- An overhaul of the Merit-Based Incentive Payment System (MIPS) that removes undue administrative and uneven financial burdens; and
- Improvements to alternative payment model (APM) options that boost physician participation in those programs.
While TMA considers those reforms top priority, it also backs a slate of related federal bills aimed largely at reducing physicians’ administrative burden within Medicare and other programs. (See “Prescription: Urgent Reform.")
“The health care marketplace is increasingly hostile to solo, small, and independent practices through factors such as low payment rates that fail to keep up with inflation; increasing administrative burdens; the inability to find and retain staff; and exclusion from health plan networks due to market consolidation and vertical integration,” states a 35-page letter TMA penned in response to CMS’ proposed 2025 Medicare Physician Fee Schedule.
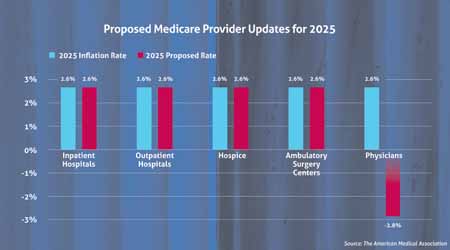
Add on yet another physician pay cut Medicare has on tap for the new year at 2.8% – while hospitals and other entities continue to receive inflationary updates – and “private practices are breaking under the pressure of lack of adequate payment and increasing overhead,” TMA President G. Ray Callas, MD, wrote in the letter.
In addition to outlining medicine’s reform plan, TMA’s lengthy comments detail a series of recommended improvements to CMS’ 2025 proposal, which includes some, albeit few, bright spots. But the annual rigamarole of an impending pay cut, a maze of MIPS changes, and the absence of permanent telehealth solutions, among other shortfalls, highlight the urgent need for relief if physician practices are to remain viable, medicine wrote.
“It’s just very frustrating because everyone [patients and physicians] is going to be affected,” Dr. Callas told Texas Medicine of Medicare’s ripple effects. For instance, private insurers use Medicare payment rates to calculate their own payment rates, so “if we don’t fix the Medicare problem and Medicare stays stagnant, or we get another cut, we’re not only losing on Medicare dollars, we’re losing on commercial rates.”
That affects physicians’ ability to care for all patients, not just Medicare patients, Dr. Callas says, urging TMA member physicians to respond to TMA’s legislative action alerts and tell federal lawmakers their story.
“Physicians’ voice is very, very big on this,” he said. “Physicians have to let their legislators know that this could be detrimental to access to care, and we’ve got to be out there and make sure that we’re educating as much as we can.”
Compounding problems
At press time, CMS was still considering public comments, and Medicare’s 2025 final physician fee schedule was expected to be released in November.
As Congress finishes its final few months of the session (which convened on Jan. 3, 2023, and is set to end Jan. 3, 2025), TMA is imploring legislators to act – with some already sponsoring reform-minded bills. The urgency for reform also comes as a key bill sponsor and ally in medicine – Texas U.S. Rep. Michael Burgess, MD (R-Lewisville), who championed the former sustainable growth rate repeal – is set to retire this month. (See “Lifelong Leadership,” Page 4, July 2024 Texas Medicine.)
According to AMA research, payment updates are proposed for nearly all Medicare entities in 2025 – inpatient and outpatient hospitals, hospice facilities, and ambulatory surgery centers, for instance – except physicians. (See “Proposed Medicare Provider Updates for 2025")
Among those practices struggling to stay viable, TMA Past President Gary Floyd, MD, points out, “we have a huge number of docs that are ages 60 to 65, who easily could retire. They managed to stay in [practice] just because they enjoy it, but if they start losing money and have to delve into retirement funds, I’m not sure many are willing to do that anymore.”
Others are shifting away from independent practice, which can leave patients with fewer access to care options, especially in rural areas as those practices feel the ongoing strain, he adds.
“We have a great environment to practice in,” Dr. Floyd said of Texas. “But if physicians can’t get paid enough to keep doors open, they’re going to look for other ways to practice.”
Medicine did welcome a handful of positive payment-related changes in the 2025 proposed fee schedule, including:
- Fixes to the evaluation and management add-on complexity code;
- Three new codes recognizing “advanced primary care management;”
- The addition of three new covered telehealth services;
- Several new codes related to behavioral health services; and
- Expanded coverage of hepatitis B vaccination, PrEP for HIV infection prevention, and colorectal cancer screenings.
But alongside payment reform, TMA overarchingly continues to advocate that CMS minimize the administrative burdens that compound physicians’ payment struggles, for example by aligning coding changes with CPT, collaborating with medicine to educate physicians on such modifications, and streamlining myriad quality measures across its value-based care programs.
“Physicians’ primary mission is to help, treat, and heal their patients who are sick and suffering, not to check boxes and chase down paperwork,” Dr. Callas wrote. TMA “urges CMS to continuously evaluate methods and policy levers that can reduce physician burnout, which leads to the unintended consequence of shortages of physicians and patient access to care.”
MIPS mess
Nor do any bright spots in CMS’ proposals overshadow what medicine’s letter described as the agency’s “failure to address the Quality Payment Program’s complexities, inconsistencies, and administrative burdens,” calling it “a devastatingly missed opportunity for the Medicare program, Medicare beneficiaries, and the physicians who care for them.”
On top of Medicare’s proposed 2.8% overall pay cut, MIPS penalties threaten to cut physician payments by up to another 9% for not meeting program requirements “with no evidence that the program supports care improvements,” TMA wrote.
Dr. Sheppard adds that MIPS continues to penalize physicians for factors beyond their control.
“If someone needs to get their mammogram, but that person has to drive three hours to go someplace that actually can do a mammogram, she may not do that. But [physicians] have no control over where the patient can get the study done,” Dr. Shepherd explained. “No one argues that we’re looking for quality, but we wanted to make sure it is fair to the physicians who are being judged on that for things that are not in their control.”
Adding insult to injury, CMS has signaled that traditional MIPS reporting will be replaced by full adoption of its newer MIPS Value Pathways (MVP) program as early as 2029.
MVP reporting is currently voluntary, and “while TMA acknowledges steps that CMS has taken to try to ease clinicians into the transition from MIPS to MVPs, TMA skeptically views the program as the same old MIPS, just rebranded and wrapped in a shiny new package,” the letter states.
Rather than force physicians into MVPs, TMA urges CMS to work with AMA’s MIPS workgroup, of which TMA is a member, and to “focus on moving physicians to risk-based systems in voluntary, physician-led alternative payment models,” as promoted in the Value in Health Care Act. Among other tenets, the bill would restore incentive payments set to expire at the end of 2024 and lower participation thresholds down from what TMA described in previous correspondence to federal lawmakers as “nearly impossible-to-reach” levels set for Jan. 1, 2025.
At the same time, TMA welcomed CMS proposals that could make it easier on low-revenue accountable care organizations with “prepaid shared savings” or advanced payments that can be invested on the front end.
Telemedicine to-dos
For physicians investing in telemedicine technology and providing such services to expand access to care, TMA also advocated in its letter they receive appropriate payment with inflationary updates, as telehealth facilities already do.
TMA continues to press Congress to make permanent payment parity for such services, so physicians are paid for in-office and telemedicine visits at the same rate, as well to permanently codify the removal of existing geographic site restrictions so patients can continue to receive care in their own home. A pandemic-era waiver allowing such flexibility expires on Dec. 31.
That waiver has been particularly helpful for patients in Texas who are mobility challenged, as well as rural patients who might live long distances from physicians but can access telemedicine services thanks to the state’s existing cell phone network and expanded broadband reach, says TMA Associate Vice President of Health Information Technology Shannon Vogel.
One telehealth-related bill before Congress would deliver that permanent waiver: The CONNECT for Health Act of 2023, introduced nearly 18 months ago in both chambers of Congress. Federal lawmakers also are considering House Resolution 7623, which would waive the geographic site restriction and allow for audio-only telemedicine visits through the end of 2026.