League City family physician Renny Varghese, MD, is often forced to find creative ways to manage his overflowing electronic health record (EHR) inbox.
From allocating specific time in between patient appointments for in-box messages to drafting “smart phrases” – sections of text inserted into patient notes or discharge instructions to summarize lab results – Dr. Varghese has become used to navigating an electronic system that “requires an incredible amount of time and energy.”
“It’s mentally draining,” the Texas Medical Association’s Committee on Health Information Technology (HIT) member told Texas Medicine. “In the last two weeks alone, I answered 445 inbox messages. It took hours of time both at the clinic and at home to address. Those hours add up to incredibly long days.”
Dr. Varghese acknowledges that electronic communication has its advantages – such as streamlined workflows and coordination of care benefits – but the mountains of notifications, refill requests, lab results, and direct messages from patients, among other alerts critical to patient care, often lead to less face-to-face patient time, he says.
Physicians are often forced to find time in their already busy schedules to clear inboxes filled with online communication. This influx can lead to increased stress among physicians and decreased career satisfaction, says Dr. Varghese. However, solutions like inbox triage, developing payment pathways for EHR work, and artificial intelligence (AI) workarounds are on the horizon.
Primary care physicians spend a median of 7.8 minutes per patient visit on EHR tasks, with chart review, documentation, and ordering functions – processes used to implement patient care, such as managing prescription requests, imaging studies, and other services – accounting for most of the time, according to a November 2023 cross-sectional study published in the Journal of the American Medical Association, “System-Level Factors and Time Spent on Electronic Health Records by Primary Care Physicians."
Although the cause of this inbox surge is multifaceted, a study published in Annals of Family Medicine found that it may be partly due to EHR tasks increasing despite in-person patient visits returning to pre-pandemic levels.
During the pandemic, when the volume of in-person patient visits declined, primary care physicians often used the extra time in their schedules to complete asynchronous patient needs in their EHRs, per the study. Now, they’ve lost the extra time, but the amount of EHR responsibilities remain.
The increase in time that physicians spend in EHRs is also significantly associated with the pandemic’s shift to telemedicine, which increased from 3.1% of medical visits to 49.3% of visits from August 2018 to September 2021, per an October 2023 JAMA study. Although the public health emergency has ended, patients continue to use telemedicine to access their doctors for some visits.
Physicians are also regularly pressed to manage excessive and unnecessary automated messages – like notifications that a patient has visited another clinician in their health system, for example – that further clog their inboxes, says Dr. Varghese, leading to more stress associated with physician burnout.
“When I was a medical student, I had no idea I’d spend so much time on messaging,” Dr. Varghese said. “It is a struggle to balance EHR [responsibilities] with patient care.”
 Strategic solutions
Strategic solutions
Medical organizations across the country are starting to address EHR-specific solutions to inbox burden, according to AMA’s resource “A System-Level Approach to EHR Inbox Reduction,” which offers guidance for reducing and streamlining inbox burden on physicians.
For instance, TMA recently took steps to address EHR burnout during the association’s annual TexMed conference in May. During the event, TMA’s House of Delegates adopted a resolution – brought forth from the Council on Socioeconomic in tandem with the HIT Committee – that sought pathways for physicians to get paid for time spent on after-hours documentation.
The policy supports:
• Increasing the relative value unit – used by Medicare, Medicaid, and insurance companies to determine how much a physician should be paid for their services based on time spent with the patient – to account for time physicians spend responding to inbox messages related to clinical care; and
• EHR vendors developing functionality to calculate the amount of time physicians spend managing the inbox both in aggregate for management purposes and per patient for billing purposes.
Other organizations are testing different solutions. The Medical Associates Clinic in Dubuque, Iowa, redelegated inbox tasks to nurses paired with a physician, allowing them to address clinical advice requests within their scope, renew medications by protocol, and perform the first review of laboratory results.
Shannon Vogel, TMA’s associate vice president of HIT, says solutions like these are becoming more common as practices begin to create “inbox task forces” among clinical staff by authorizing a common in-basket where the care team, led by a physician, can triage messages.
Houston internist Gary Sheppard, MD, endorses the triage method and regularly delegates inbox responsibility to appropriate staff members. However, what he calls his “hyper-focused” approach to EHR management doesn’t stop there.
The chair of TMA’s Council on Socioeconomics also suggests physicians cultivate an open line of communication with EHR vendors and actively seek the right system for their practice – a tip he suggests after switching to a new EHR vendor in May.
TMA members can use TMA’s EHR Comparison Tool to help identify product features, functionality, and pricing that will best suit their practice.
Dr. Sheppard also recommends physicians create inbox protocols with their staff, a suggestion that aligns with AMA’s STEPS Forward toolkit that offers systematic approaches to reducing EHR inbox burden.
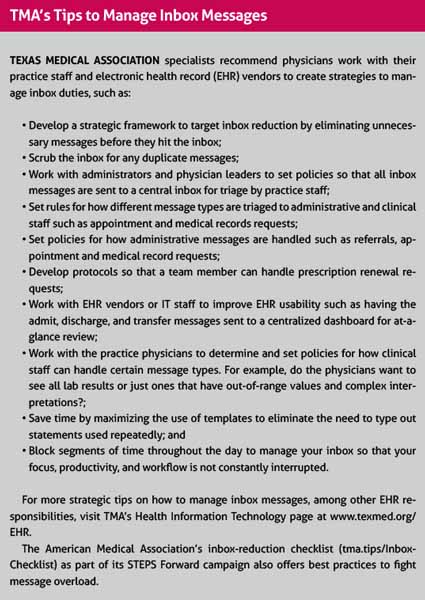
TMA has educational resources available to aid physicians in finding inbox solutions that work for their practices, from the association’s EHR comparison tool to its telemedicine resources. (See “TMA’s Tips to Manage Inbox Messages,” left.)
Dr. Sheppard believes TMA and other groups in organized medicine are “essential” to fighting the ever-increasing electronic burden.
“What works for one practice may not work for every practice, but it is important for every physician to seek solutions that work for them,” Dr. Sheppard told Texas Medicine.
Augmented answers
Dr. Varghese has turned to another solution for inbox management – AI. He uses EHR-integrated, AI speech recognition software to draft patient documentation like appointment summaries and refill requests, and by avoiding typing his notes, he’s able to shave minutes from daily EHR work to spend more meaningful time with his patients, away from screens.
Dr. Varghese’s use of AI mirrors TMA’s 2022 policy, which specifies, in health care, TMA prefers the term “augmented intelligence” over “artificial intelligence” as the former implies it supplements human decision-making and should not be used to replace physician reasoning and knowledge. As such, TMA’s policy supports the use of AI when used to support physician decision-making, enhance patient care, and improve public health, among various other principles. AI technology has been integrated into multiple EHR systems and have chatbot-based platforms that can format clinical documentation and common medical correspondence, among other benefits.
According to AMA, AI can also:
• Reduce the amount of pajama time physicians face;
• Automate workflows; and
• Personalize and improve the usability of EHR systems.
Dr. Varghese said many of his patients are quick to send messages through their patient portal about new or ongoing symptoms for advice “right away” – even if those symptoms are not urgent and can be addressed during their next visit.
He says AI is helpful when aiming to deliver timely message responses to patients who’ve become used to instant gratification offered by smart phones.
By using AI, Dr. Varghese has been able to respond to patients quicker. However, he says the most impactful way physicians can reduce messaging is simply by speaking to their patients about proper inbox usage.
“Patients are used to instant responses and expect nothing less from their doctors,” he said. “But they also just don’t understand that physicians have a heavy workload that keeps them from responding. A very easy way to reduce how often patients message us is by clarifying appropriate messaging.”
Dr. Varghese adds that it’s important to “stay positive.”
“Just accepting that I’m doing as much as I can helps me to avoid becoming overwhelmed,” he said. “I’ve learned to let go of the idea that I need to be perfect.”