Following strong pushback from the Texas Medical Association, UnitedHealthcare (UHC) has effectively reversed its payment-cutting policy change on “incident-to” billing for services performed by nonphysician practitioners (NPPs).
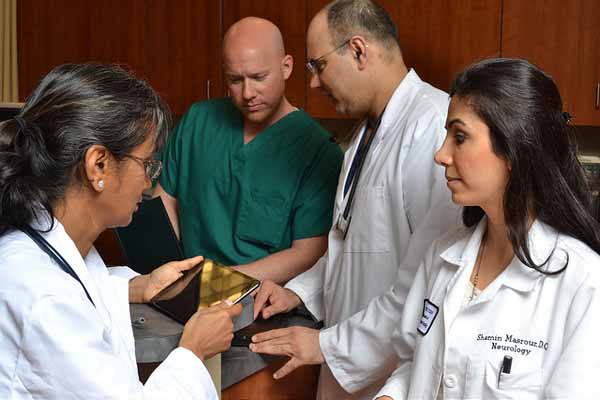
Like Medicare, a number of commercial plans allow practices to bill insurers for physician-directed, NPP-performed services at the full payment rate for physicians, as long as certain requirements are met. TMA believes incident-to billing boosts access to care by allowing physicians and NPPs to collectively see more patients through a team-based approach.
But a UHC policy change scheduled to begin May 1, 2021, threatened to curb that long-standing billing practice by requiring nurse practitioners, physician assistants (PAs), and clinical nurse specialists to use their own National Provider Identifier (NPI) number when billing. Depending on a practice’s contract, the change could cause a 15% payment reduction for those services.
TMA strenuously objected to the change both during and after the implementation date. Among other points, TMA cited the confusion and financial concerns it would cause during a public health emergency.
This week, UHC posted a new incident-to policy that walked back the previous requirement to use the nonphysician’s NPI number.
As of Aug. 1, the policy says, UHC considers incident-to services payable “if the services are rendered by an advanced practice health care or nonphysician practitioner” and the services are:
An “integral, although incidental” part of the supervising physician’s services;
Commonly rendered free of charge or included in the supervising physician’s bill;
Putting the final nail in the coffin of its previous policy announcement, UHC says services that meet the incident-to criteria “should be reported under the supervising health care provider’s NPI number.”
TMA President E. Linda Villarreal, MD, calls UHC’s reversal a win for organized medicine. In June, the American Medical Association adopted a TMA-supported resolution that called on medicine to advocate against any efforts by payers – private or public – to eliminate incident-to billing.
“Both entities have believed that it was a very bad idea to begin with, and it really impacted our whole concept of a team-based environment within the physician office,” Dr. Villarreal said. “Unfortunately, because of the shortage of physicians in general, the lack of payment to physicians to be able to sustain their practice requires additional patient volumes. You can’t do that without a team-based practice, which includes our nurse practitioners and our PAs.”
A 15% payment cut on incident-to services would have sizable ramifications, she adds.
“The payment for physician care does not fit the bill already. So, to decrease it by 15%, multiply it by 100 or 1,000 or however you want to look at it, it’s a significant impact,” she said. “It could involve less hours at a physician practice. It could involve having to have a staff member let go.”
TMA and other physician organizations will meet with UHC later this month to collect more information on the policy change, including how the insurer is handling claims submitted between May and the end of July.
To help physicians navigate the complicated pitfalls of incident-to billing, TMA has produced an education sheet on basic guidelines and requirements.
And on Aug. 17 at noon CT, TMA will host an Ask the Expert virtual session titled Nonphysician Practitioners and Scope of Practice, which will teach participants how to comply with state laws and regulations on delegating and supervising prescriptive authority. Register now.