
Physician well-being, which was at a crisis point heading into the COVID-19 pandemic, has only deteriorated since early 2020. But the Texas Medical Association and county medical societies are on the front lines, working together to support physicians as they contend with burnout, financial stress, and administrative burdens exacerbated by the public health emergency.
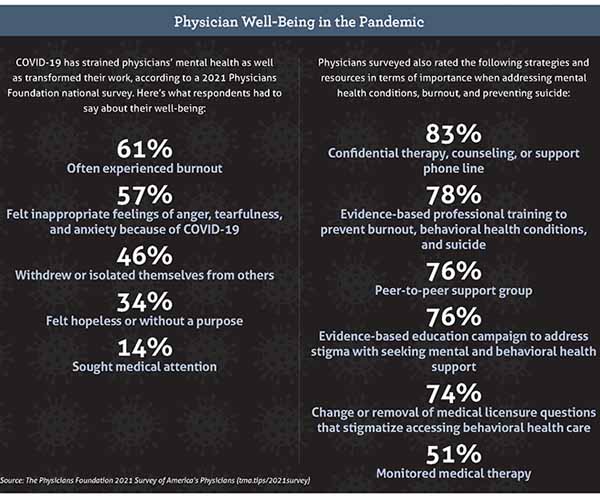
Nearly two-thirds of physicians – 61% – experience burnout, and more than half – 55% – know of a physician who has considered, attempted, or died by suicide, according to a 2021 national survey conducted by The Physicians Foundation (tma.tips/2021survey). By comparison, 40% of 2018 survey respondents said they often or always experienced burnout, which was then an all-time high.
Aware of these concerning trends and the added pressures of the pandemic, the TMA Foundation applied for and received a $75,000 grant from the Pfizer Foundation, which it used to establish the Caring for Physician Healers: Mental Health and Wellness Resources During COVID-19 Fund in fall 2020. Since then, the fund has awarded grants to seven county medical societies, five of which started new physician wellness programs. (See “Resources,” page 24.)
Such efforts are desperately needed: Only about a dozen of the 112 county medical societies chartered by TMA currently offer physician wellness programs, according to TMA staff. The pandemic also has added new challenges, including surging hospitalizations, rampant misinformation, and widespread staffing shortages.
“The impact of COVID-19 on medical professionals is multifold and reverberating,” said Sejal S. Mehta, MD, a Plano psychiatrist who chairs TMA’s Committee on Physician Health and Wellness. “Medical education has become more complicated, the health care delivery system is strained, and physical and emotional well being is being tested.”
Setting an example at the county level
In early 2021, the Travis County Medical Society (TCMS) saw a sharp increase in use of its free and anonymous Safe Harbor Counseling program, which gained 71 new clients through mid-September and nearly doubled its number of monthly appointments.
“The good thing that has come of this is that physicians in our community are more likely to reach out for help now,” said Brian Sayers, MD, an Austin rheumatologist who chairs TCMS’ Physician Wellness Program.
TCMS, one of the TMAF grant recipients, launched its physician wellness program in 2017. The year prior, Chief Operations Officer Belinda Clare had learned of a physician wellness program in Oregon founded after three physicians in the Eugene area died by suicide in an 18-month period. Inspired to prevent a similar tragedy in Travis County, she and Dr. Sayers took the idea to the TCMS board, which embraced it. Today, the program includes a confidential counseling service that has provided about 1,000 visits, educational resources, events, and a blog.
County medical societies are well suited to provide such support because of the trust they build with members. Many health systems and other employers offer employee assistance programs, which provide free and confidential assessments, short-term counseling, referrals, and follow-up services for personal and work-related problems. But physicians often eschew such benefits out of fear that doing so will affect their career or carry a stigma, Ms. Clare says.
To avoid this same outcome, TCMS set up its own counseling service to be completely anonymous and extends the benefits to members’ spouses. It also vets the psychologists who serve as counselors and pays for the first four sessions, which has been especially important during the pandemic, when many physicians have struggled financially.
“We do all the legwork,” Ms. Clare said.
Dr. Sayers makes sure to promote the counseling service in his weekly emails.
“There’s a lot of suffering going on out there, and we just really feel as a family of physicians that we need to be discussing mental health openly and constantly,” he said.
The vital service is expensive. Dr. Sayers estimates that it has cost TCMS close to $200,000 since its inception. But he encourages other county medical societies that are interested in starting a physician wellness program not to get spooked by the expense, citing buy-in from hospital systems, large clinics, and member physicians. In fact, TCMS developed the LifeBridge Physician Wellness Program Tool Kit – a free 132-page guide – to help other organizations replicate its success (tma.tips/lifebridgetoolkit).
“People really express how much this has helped us as a physician community,” Dr. Sayers said.
The Dallas County Medical Society (DCMS) has taken a slightly different approach to the same issue. Early this year, CEO Jon Roth was watching the morning news and saw a segment about the Emotional PPE Project, a national effort to connect health care workers to volunteer mental health counselors free of charge.
The timing was fortuitous. As in Travis County, many physicians in the Dallas area were struggling with the pandemic amid the holiday surge. By the end of 2020, more DCMS member physicians had retired than in any of the previous five years. Mr. Roth also started to notice a sense of fatigue while on Zoom calls and a new edge to many members’ voices.
“It’s kind of like when you see it, you know it,” he said.
Using TMAF grant funding, DCMS partnered with the Emotional PPE Project in January. Because DCMS can promote the initiative to its membership, and because the Emotional PPE Project can provide access to its network of volunteer counselors, the program has low overhead. Mr. Roth expects it to continue through at least the end of the pandemic.
More importantly, physicians are taking advantage of this new resource. Although the Emotional PPE Project does not provide exact numbers to preserve users’ confidentiality, Mr. Roth says it has seen a fourfold increase in demand across the Dallas area since partnering with DCMS.
“We know we’re having some effect,” he said.
Investing in the future
After a series of physician suicides at Houston-area hospital systems, the Harris County Medical Society (HCMS) launched its own physician wellness program in 2018. It includes a network of 15 psychologists and psychiatrists who can meet with high-risk members within 72 hours; seminars and events; practice management support; educational resources; and member discounts at Houston-area attractions.
“Everyone has a different way that they unwind. So, we need to be broad and comprehensive in how we respond,” then-HCMS Executive Vice President and CEO Greg Bernica said.
This comprehensive programming has proven useful during the pandemic, especially during the last few months, as the delta variant and low vaccination rate have overwhelmed Texas hospitals. Like other programs, HCMS has seen a recent uptick in demand from its 12,500 members. Its physician wellness webpage saw double the number of views between January and September compared with the same period last year.
“It’s worse now,” Mr. Bernica said of the pandemic’s impact on physician wellness. “[Physicians] are seeing all this death in the ICUs, and it shouldn’t be happening.”
A key component of HCMS’ program is its outreach to area health systems and medical schools. Together, they can pool their resources, promote each other’s services, and reach a wider audience. Although the pandemic has caused some delays, Mr. Bernica says nearby institutions have embraced this collaboration and share HCMS’ commitment to battling burnout and preventing suicides.
“From an institutional standpoint, it’s very expensive to replace a physician,” he said.
The loss of any physician – to another field, early retirement, or death – is also disastrous for Texas. The state’s physician shortage is expected to grow to 10,330 by 2032, up from 6,218 in 2018, according to the Texas Health and Human Services Commission. Meanwhile, the state currently spends $45,733 per medical student per year, or almost $183,000 over four years.
Investing in physician wellness serves not only HCMS’ members but also the entire heath care ecosystem in the Houston area – and beyond.
“We need them there for their patients,” Mr. Bernica said.
Tex Med. 2021;117(11):22-25
November 2021 Texas Medicine Contents
Texas Medicine Main Page