Texarkana internist Dewitt C. “Charles” Fortenberry, MD, is used to navigating complex billing challenges.
Located on the Texas-Arkansas border, Dr. Fortenberry treats patients from both states and even some from Oklahoma, bringing unique payment issues to his doorstep.
“I’m proud to treat patients from multiple states, but receiving timely and accurate payment for their appointments has been tricky,” he said. “Payers aren’t forthcoming communicators, especially about denials or how to appeal them. It’s often felt like wandering through the dark.”
Unsure of how to maneuver unresponsive health plans, Dr. Fortenberry turned to the Texas Medical Association’s free Physician Payment Resource Center (PPRC) in the hope that TMA experts could “speak payers’ language.”
To his surprise, Carra Benson, TMA’s director of reimbursement services, drove five hours to visit his practice in Texarkana. During her visit, Ms. Benson identified common communication and credentialing missteps behind payment denials; worked with his billing manager to build a system for their practice to follow up on claims after they’re filed; and provided Dr. Fortenberry with practice tips to avoid those issues in the future.
“Her suggestions – like implementing checks and balances that allow me to keep track of my claims – enabled increased insight into what may have fallen behind or why a claim was returned unpaid,” he said. “This allowed my staff to then immediately refile or fix those claims with that knowledge in mind.”
But she didn’t stop there, Dr. Fortenberry says.
“Not only did Ms. Benson provide concrete solutions to billing mistakes on our end, she also directly spoke to payers to advocate for my practice,” he said. “Let’s face it, I don’t have the time or even the expertise to get into conversations with payers who seem to speak a different language – but TMA specialists speak that language.”
Payment advocacy
Originally named the Hassle Factor Log, TMA’s PPRC service began in 1989 in response to efforts by then-Medicare contractor Blue Cross and Blue Shield to recoup overpayments made to Texas physicians.
In response, TMA’s Council on Socioeconomics formalized TMA’s program the next year, setting four objectives:
- Identify physician time and effort wasted by insurance hassles;
- Specify bureaucratic abuses that occur in the claims systems;
- Find ways to eliminate administrative burdens on physicians; and
- Provide a factual basis for advocacy efforts designed to achieve those ends.
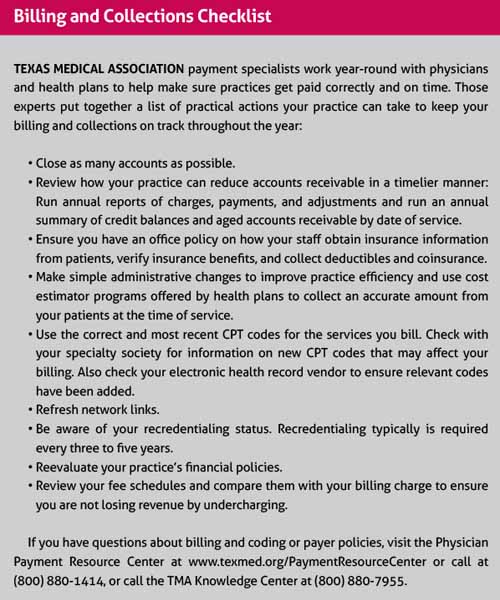
Since then, PPRC staff experts have gone to bat for members by helping their practices resolve issues related to insurance payments – including payer network status, prompt pay, and other payment and claims issues – and by regularly meeting with payers to discuss physician concerns.
“It’s easy to forget how much advocacy goes into these carrier meetings,” Ms. Benson said. “We make sure that we understand what issues physicians are dealing with so we can bring solutions to their practice, and to payers. This is the vehicle of PPRC’s advocacy.”
PPRC specialists meet directly with Medicare, Medicaid, large private payers, and other health plans to discuss specific issues that cause lost revenue for physicians. In 2023, TMA recovered more than $3.6 million for Texas practices.
An open door
Austin neurologist Jerald Simmons, MD, was one of those physicians.
“For what felt like no reason at all, an insurer updated their policies to exclude medical devices necessary to treating sleep disorders at home,” he said. “I was so upset, I contacted the health plan for answers, but I couldn’t get through to anyone. That’s when I reached out to TMA.”
Dr. Simmons’ practice heard back from the health plan within a day of TMA experts advocating directly to the payer and, after that conversation, found the plan had reviewed its policy and reversed the decision.
“That harmful policy may still be in place if not for TMA staff,” he said. “I’m thankful they were here to confront payers with how their decisions could harm patient care.”
Similarly, Dr. Fortenberry saw improved communication from payers and fewer payment denials within a few months of TMA’s visit. That aid was especially critical as Dr. Fortenberry’s practice evolved.
When he began treating older patients enrolled in Medicare and Medicaid and living in nursing homes, he had trouble receiving payment at one of those homes.
“So, [Ms. Benson] spoke to my enrollment and credentialing experts to ensure my practice was properly credentialed. Once we were, delayed payment came in. We would not have been able to get paid at all if [Ms. Benson] hadn’t figured Medicaid and Medicare enrollment out.”
TMA experts continue to work with Dr. Fortenberry’s practice as new concerns arise.
“We’re still working out some billing kinks, but I feel so much more confident,” he said. “The great thing about working with TMA staff is that they didn’t just make their recommendations and then disappear. Their involvement has been an open door. We still communicate from time to time when other hiccups have come up, and they’ve been very helpful in helping us to resolve those issues.”
Through the Council on Socioeconomics, TMA continues to meet with all five major health plans – Aetna, Humana, UnitedHealthcare, Blue Cross and Blue Shield of Texas, Inc., and Cigna – to discuss physician payment challenges.
“TMA represents physicians so that we experience much more [progress] with these big payers,” Dr. Fortenberry said. “For years, I felt like I was being ignored. TMA throws weight behind my requests, and because of that, I have a lot better chance to getting these kinds of issues resolved.”