In April 2020, aerial photos of a packed food bank parking lot in San Antonio made national news, highlighting the issue of food insecurity during the early months of the COVID-19 pandemic.
Nearby, Woodson “Scott” Jones, MD, a pediatrician and vice dean for graduate medical education at the UT Health San Antonio Long School of Medicine, took notice.
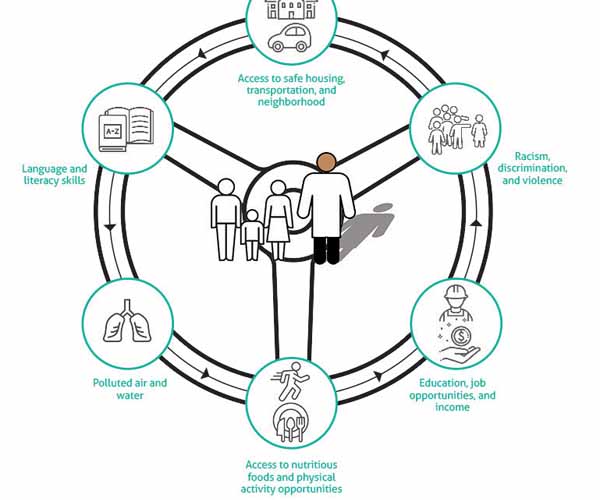
In conjunction with patient visits, the photos spurred Dr. Jones and the Long School of Medicine to address nonmedical drivers of health – the conditions in which patients live, work, and play – head on.
“We saw firsthand how these [nonmedical factors], from food to transportation [and] lack of ... insurance, were impacting their health,” he told Texas Medicine. “It became really real for us.”
So, in 2022, the Long School of Medicine, along with its parent organization, The University of Texas Health Science Center at San Antonio, debuted an annual one-day training event on nonmedical drivers for medical residents during orientation.
The training teaches residents about nonmedical factors, related screening tools, and community resources that can help patients in need. The focus: awareness, says Dr. Jones, who serves on the Texas Medical Association’s Council on Medical Education.
Like many physician practices that have tried to address such outside impacts on patients, UT Health San Antonio has run into a host of challenges related to the training, including residents’ jam-packed schedules.
More broadly, health plans rarely pay residents and physicians for this kind of screening, disincentivizing more widespread adoption. Practices that do screen for nonmedical factors often struggle to connect patients who screen positive to community resources given the staff and infrastructure necessary to do so; those that are successful often see patients disregard such referrals for myriad reasons. (See “Quality of Life,” July 2023 Texas Medicine, pages 26-29.)
But this tide may be changing. On both the state and the federal levels, there’s a shift toward value-based care models, which incentivize preventive care and, often, health equity, as well as increasing adoption of related screening tools. Heeding TMA physician advocacy, the 2024 Medicare Physician Fee Schedule also implemented a new “G” code to pay clinicians for screening eligible patients for certain nonmedical drivers, including housing insecurity, food insecurity, transportation needs, and utility difficulty.
TMA continues to monitor these developments and to educate its member physicians about them.
For Dr. Jones, screening is a crucial step toward valuing physicians’ role in addressing nonmedical factors and, in turn, strengthening patients’ access to care, improving their health outcomes, and reducing health care spending.
When this happens, residents at the Long School of Medicine will be ready.
“The nexus is now,” he said. “The stars are aligning.”
The medical school will host its third annual nonmedical drivers of health residency training this June, building on past events and community needs. In the meantime, UT Health San Antonio is incorporating nonmedical drivers-related education in other ways, given resident interest.
Averi White, MD, internal medicine chief resident for quality and safety at UT Health San Antonio, spoke to residents during the 2023 training about her own experience with nonmedical drivers. As a first-year resident during the height of the pandemic, Dr. White learned she could stave off burnout by learning more about her patients than their ventilator settings and medication doses. For instance, a patient with hypertension may be struggling with his diet because his wife, who cooked all his meals, recently died, leaving him reliant on fast food. “We have a responsibility when we practice medicine ... to love humanity as well, and, to me, that’s what [nonmedical drivers are],” she said.
The 2024 training will include more community resources, including those focused on asthma and diabetes, both of which are common among San Antonians. The Long School of Medicine also has partnered with the city’s public health department, Metro Health, and its Healthy Neighborhoods program, which helps develop individualized community health action plans.
Dr. Jones says such partnerships build community awareness of UT Health San Antonio’s efforts to address nonmedical factors as well as residents’ awareness of community resources.
Yet another barrier is ensuring patients, once connected to resources, benefit from them.
“The big unanswered question is, ‘When we make them aware of these resources, are they actually taking advantage of them?’” Dr. Jones said.
In an attempt to answer, UT Health San Antonio has developed a suite of other residency training opportunities. These include the family medicine “promotores” program, which relies on community health workers, or promotores, to build trust between resident physicians and their patients, as well as the Continuity Clinic, staffed by pediatric residents who screen patients for nonmedical drivers.
Since 2021, UT Health San Antonio also has offered an internal medicine health equity track, which teaches residents to understand nonmedical drivers and “to act as partners for improved living conditions, health literacy, and access to services,” according to the program syllabus.
Dr. Jones sees the track as a jumping-off point for more longitudinal resident training on nonmedical drivers.
“That track ... really is preliminary for what we hope will cross over to multiple programs, and that’s because residents are asking for it,” he said.
Like these San Antonio residents, physicians across Texas are grappling with how to address nonmedical drivers of health in their own patient populations, and TMA is dedicated to helping them do so.
For instance, TMA’s Council on Health Care Quality is developing a free CME webinar to help member physicians implement such screening tools and access payment for using them, due this fall.
As the impetus for the CME, Ajay Gupta, MD, a family physician in Austin who chairs the council, points to prioritization of specific quality measures related to nonmedical drivers by the Centers for Medicare & Medicaid Services and the National Quality Foundation. (See “Closing the Loop,” May 2022 Texas Medicine, pages 22-25.)
“We want to make sure that the [TMA] membership is aware of this,” he said, adding that he hopes physicians adopt such measures given the outsized role they play in patient health outcomes.
TMA also is involved in data collection efforts, including the Texas All-Payor Claims Database. The Texas Legislature established the TMA-backed database during the 2021 session; still in development, it will collect public and private health insurance claims with the goal of improving state population health. (See “Power Data,” March 2022 Texas Medicine, pages 36-37.)
Although not explicitly focused on nonmedical drivers, the database might improve patients’ access to care by improving price transparency, reducing cost variation, and supporting a more competitive marketplace, says TMA President Rick Snyder, MD, a cardiologist in Dallas who represents TMA on the database advisory group. He adds that researchers also might use the database to elucidate which nonmedical drivers are impacting Texans’ health outcomes and why.
“It’s all about improving quality, reducing cost, and, especially, promoting affordability of health care,” he said.