
Bridge City family physician Amy Townsend, MD, transitioned from hospital-based care to direct primary care in 2020 after “contemplating leaving medicine altogether.”
She felt the weight of financial strain, a heavy administrative workload, and a lack of clinical autonomy prevented her from making independent decisions about her patients’ care.
Unwilling to compromise any longer, Dr. Townsend opened her own practice to “reconnect to the patient-physician relationship” and to claim full authority over the care she provided, from what medication she prescribed to what appointment options she offered.
“The environment I used to practice in did not allow me to provide care the way I wanted to. I had minimal freedom to make what I considered the best decisions for my patients, free from outside constraints,” she told Texas Medicine. “When I started my own practice, I could finally become the type of physician that I’ve always wanted to be.”
Dr. Townsend calls her switch “lifesaving.” However, she acknowledges she now faces unique challenges to her private practice, like economic consolidation, increased costs, and what she describes as “systemic flaws” that allow Medicare to pay hospitals more than physician-owned practices.
That gap has continually widened with Medicare physician pay declining 29% from 2001 to 2024, even as the cost of providing medical care has increased with inflation, per March research from the American Medical Association. Payments to hospitals and other entities, meanwhile, have kept pace.
Since 2000, for example, the price of services, insurance, medication, and medical equipment has increased by 119.2%. In contrast, prices for consumer goods and services rose by 85% in the same period, according to a May study by the Peterson Center on Healthcare and Kaiser Family Foundation.
A January 2021 Health Services Research study showed Medicare payment for services provided by physicians working for a hospital or health system is significantly higher than that paid to independent physicians for the same services. Integrated hospital systems have the potential to see $114,000 more in Medicare payment per physician annually than independent practices, researchers found.
Dr. Townsend says these payment disparities, among other issues that plague private practice, create barriers for physicians to compete with hospital-owned facilities, large groups, or for-profit clinics owned by non-health care entities.
“It often feels like there’s no room for the independent physician,” she said.
Still, Dr. Townsend and others in private practice are finding ways to navigate those challenges.
For example, Dr. Townsend’s primary care practice allows her patients to purchase a membership that grants unlimited access to certain primary care services – like routine screenings and acute-care visits – directly from her practice without having to file an insurance claim. The patient pays a monthly fee to access care as needed, without having to make an additional payment at the time of service.
This helps Dr. Townsend navigate costs “her way,” she said. “I rediscovered my love for medicine after finding the right health care model that met both my and my patients’ needs. I don’t want any physician to forget that they have options, even when things look bleak.”
Rising to the challenge
An April 2024 report by the Physicians Advocacy Institute (PAI) and Avalere Health found the majority of physicians are now in employed settings.
This reality spurred TMA to develop targeted resources to help physicians across specialties, practice settings, and payment models through its new standing Committee on Independent Physician Practice, to be led by Dr. Townsend and Austin ophthalmologist Michelle Berger, MD (See “Committee on Independent Physicians Practice Announce Members,” page 48.)
The new 15-member committee, which takes on the mantle of its predecessor, the Ad Hoc Committee on Independent Physician Practice, will help identify the needs of independent physicians and the related services that TMA may develop to address those needs. That includes:
- Identifying challenges to viability of private practice in Texas; and
- Developing and recommending policies and association resources to support the viability of independent physician practices.
The committee also will provide resources for students, residents, and young physicians who are interested in private practice but who may worry about whether it’s a sound financial decision.
“My hope is that this committee will help TMA support the viability of private practice, increase advocacy in this area, and let other independent physicians know that our association is listening to their concerns,” said Dr. Townsend, the committee’s vice chair.
As chair of the committee, Dr. Berger plans to use her decades of experience as both a TMA leader and privately practicing physician to aid colleagues as they face complexities she calls “all too familiar.”
This year, Dr. Berger says she was forced to close her practice’s doors after the February Change Healthcare cyberattack left her without claims payments for months. However, the attack was but one of many obstacles she says challenged her practice for years. For example, prior to closing her practice, she witnessed growing health care consolidation – caused in part by inflation and rising costs – often force physicians to move to employed settings as larger practices have more leverage when negotiating with health plans.
Large groups also have greater potential to gain the financial rewards of new payment models, she says, such as value-based care arrangements. (See “Value Proposition,” page 30.) These models typically require steep start-up investments in technology, case managers, and data analytics – tasks that solo and small practices often cannot add to their already heavy workloads as they contend with market forces like worsening administrative burdens, prior authorization hurdles, and a tight labor market.
Some of these trends have led 72% of Texas physicians to employed settings – like hospitals, health systems, or other corporate entities – while 28% remain in independent settings, according to PAI and Avalere Health. (See “Tracking Texas Physicians,” page 28.)
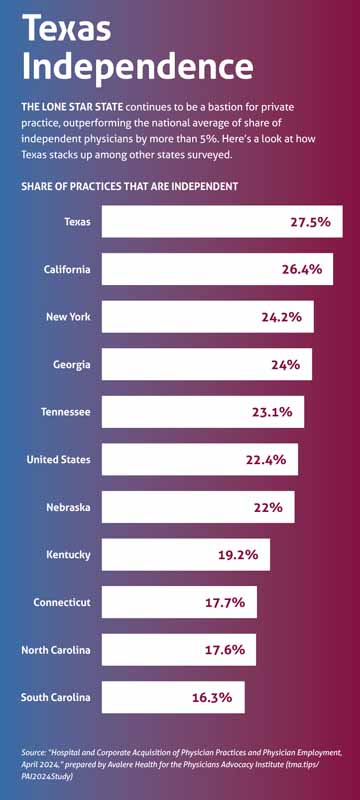
However, Texas remains a stronghold for independent practice, says TMA CEO Michael Darrouzet, vice president of the PAI board. The institute’s latest report shows Texas has a higher percentage of independent physicians than the national average, despite that number steadily decreasing since 2019. (See “Texas Independence,” page 19.)
“There are many independent doctors in Texas that are … happy to fight the battle [for private practice], and we [TMA] want to say we are here for them,” Mr. Darrouzet told Texas Medicine.
Dr. Berger says her experience has only reinforced her desire to see TMA uplift fellow independent doctors and to share their experiences with other Texas clinicians.
Thus, the new committee will aim to support physicians across the practice-setting spectrum, whether established and struggling to stay afloat or seeking an alternative, with a “strong voice” for private practice, she said. “I would scream it from the rooftops if I could. We are here, we are here, we are here.”
Hearing physician concerns
Marble Falls ophthalmologist Kelly Green, MD, says the steady decline of independent physician practices – and the acquisition of those practices by hospitals, payers, and private equity groups that, in turn, may have the market power to command higher prices – is “not in patients’ best interests.”
“These settings often view patients as a product, with a dollar sign above their head,” she said.
She adds that fewer independent practices can mean less choice for patients. For example, a patient who has an appointment with a primary care physician employed by a hospital may not receive referrals to specialists who are not employed by that hospital.
This can result in a closed-loop system of care that could “line the hospital’s pockets,” Dr. Green says.
However, she is hopeful about several ways lawmakers and physicians can ensure the viability of independent physician practices and create a competitive marketplace for both doctors and patients.
First, she says, Congress can fix how Medicare pays doctors. Without a remedy, some physicians may reexamine other career paths, especially as problems like prior authorization dramatically increase practice hassles.
“In my ideal world, every physician would get paid [appropriately] for the work they do,” she said.
A U.S. House of Representatives committee recently examined solutions like Dr. Green’s.
In a May 23 hearing, “The Collapse of Private Practice: Examining the Challenges Facing Independent Medicine,” the House Committee on Ways and Means Health Subcommittee discussed reforming Medicare payment, reducing administrative hurdles like prior auth, and improving access to care – solutions TMA has long advocated for via several pieces of legislation.
At the top of that slate, the Strengthening Medicare for Patients and Providers Act, House Resolution 2474, would ensure physicians receive inflationary updates, just like other Medicare clinicians receive.
“Financially, the source of revenue for [physicians] is fixed, decreasing, and largely not in their control. Congress not dealing with the annual issue of Medicare pay cuts to physicians, and lack of permanent payment reform, has exhausted an already burned-out population of physicians,” Chris Kean, Chief Operating Officer of TSAOG Orthopaedics & Spine in San Antonio, said during the hearing.
She highlighted several challenges facing independent physicians, such as:
- Financial strain, citing “unsustainable” payment reductions;
- A shift in control over health care decisions and delivery from physicians to insurance carriers and corporate shareholders; and
- Rising costs stemming from a consolidated health care system that allows salary rates to become significantly higher than the market average.
As for prior authorization, it “has been an absolute disaster,” Ms. Kean told lawmakers. “It does absolutely nothing to improve care, but it does allow insurance carriers to deny care.”
Ms. Kean testified on behalf of independent physician struggles after years of watching her group “struggle with or lose the battle” for private practice, she later told Texas Medicine. “Independent physicians are in the trenches.”
In a June 6 comment letter to the subcommittee, developed with input from the new Committee on Independent Physician Practice, TMA called for additional solutions to longstanding physician burdens, like cyberattacks, burnout, and staffing shortages.
“As Congress further explores challenges that threaten the independent practice of medicine, TMA asks you to consider the consequences of payment reductions, administrative complexities, and the impact of the health insurance market and hospital consolidation on small, solo, and often rural practices. TMA asserts that inaction will accelerate the decrease in independent physician practice across the United States, ultimately reducing care and increasing costs for patients,” TMA President G. Ray Callas, MD, wrote.
He went on to caution that “Physicians have an ethical duty to their patients, whereas corporate boards of directors and officers have fiduciary duties to shareholders and the corporation itself. Often corporate entities consider independent physician practices to be competition, rather than partners in providing health care in their community. As such, TMA sincerely appreciates congressional leaders examining the financial and regulatory burdens facing independent medical providers and how continued challenges result in consolidated health care systems and barriers to patient care.”
In addition to Medicare payment reform, TMA strongly supports a slate of bills that would prop up physician practices including:
- The recently re-introduced, bicameral and bipartisan Improving Seniors’ Timely Access to Care Act, House Resolution 8702 (Senate companion bill is SB 4532), which would streamline and standardize the use of prior authorization within Medicare Advantage via an electronic process and increase transparency requirements for health plans.
- The bipartisan No Fees for EFTs Act, House Resolution 6487, which would prohibit payers from imposing fees on practices that use electronic funds transfers to receive payment.
- The Patient Access to Higher Quality Health Care Act, House Resolution 977 by U.S. Rep. Michael Burgess (R-Texas), which would overturn the federal ban on creating and expanding physician-owned hospitals.
“Physicians are in the best position to make decisions with and for their patients, so it’s not surprising that Congress is considering allowing new physician-owned hospitals that align the interests of ownership and practicing physicians to improve patients’ care,” Mr. Darrouzet said when HR 977 was first introduced in Feb. 2023.
TMA also addressed challenges independent physician practices face in complying with burdensome requirements associated with the Merit-Based Incentive Payment System (MIPS), calling on Congress to work with physician associations to:
- Mitigate steep MIPS penalties that disproportionately harm small, rural, independent practices and practices that care for the underserved.
- Hold CMS accountable for timely and actionable MIPS and claims data, as required under MACRA.
- Make MIPS more clinically relevant and less burdensome.
At the state level, TMA continues to prioritize physician autonomy and corporate practice protections with related wins during the 2023 regular legislative session.
On the community level, Dr. Green strongly encourages independent physicians to mentor medical students and residents interested in private practice.
“If you want to see more students enter private practice after training, you need to show them how,” she said. “Alone, we’re just one doctor. Together, we’re a voice for independent practice in Texas.”