In a hearing packed with representatives from medicine, nursing, pharmacy, behavioral health, licensing boards, and academia, the Senate Health and Human Services Committee tackled Texas’ health care workforce shortages with the Texas Medical Association delivering its message loud and clear: Expanding scope of practice is not the answer to helping patients in rural and underserved areas.
Access to care is one of dozens of priorities for the 2025 legislative session announced by Lt. Gov. Dan Patrick this past spring. In the run-up, the Senate committee is charged with examining “whether regulatory and licensing flexibilities could improve access to care, particularly in medically underserved areas of Texas” and making recommendations, if any, “to improve access to care while maintaining patient safety.”
“This is a scope conversation,” committee Chair Sen. Lois Kolkhorst (R-Brenham) said in laying the foundation for several extensive panels held Sept. 18, adding that the committee is looking for a “balanced approach.”
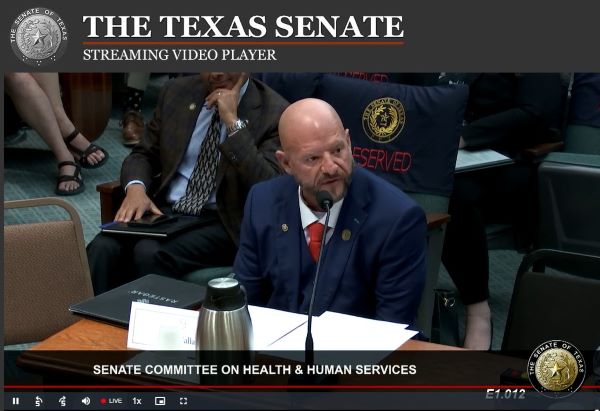
That’s exactly what stakeholders achieved a decade ago when the Texas Legislature approved the state’s current framework for physician-led team-based care, which still works to protect patients, TMA President G. Ray Callas, MD, testified.
That framework “aims to ensure Texans receive care by licensed physicians who have completed the necessary training of medical school, residencies, and fellowships to lead the health care team. When seeking to address access to care, the last thing we want to do is to lower the standards under this well-constructed framework, or to jeopardize patient care,” he said in prepared testimony. “Texas’ physician-led team-based care models promote oversight and collaboration while keeping patient safety the priority.”
Dr. Callas pointed to several studies showing nurse practitioners prescribe more, order more tests, have higher referral and hospitalization rates, and perform more poorly on quality measures than physicians – all of which can lead to greater patient safety risks and health care costs. He highlighted additional research on the inconsistent quality of nursing education programs and maldistribution of nurses, who tend to practice in the same areas as physicians, regardless of scope-of-practice laws.
On behalf of the Texas Medical Board, its president Sherif Zaafran, MD, elaborated on the differences between physician and nurse training and the collaborative nature of Texas’ supervision and delegation structure, saying it “maximizes the strengths of each team member.”
Given the inherent complexities of patient care, “there should be an evidence-based focus on ensuring access to quality health care rather than a focus on shortages and distributions,” he said.
An expert invited on behalf of medicine also debunked nonphysicians advocates’ arguments that scope-of-practice expansions save costs with little risk. Ft. Myers, Fla., family physician Rebekah Bernard, MD, author of Imposter Doctors: Patients at Risk who has researched and written on scope of practice, echoed TMA testimony cautioning about the invasion of corporate interests into medicine simply to save money over ensuring care quality.
The decades of published research showing nurses can provide great care "involved nurse practitioners working under physician supervision following physician-created protocols or treating low-risk patients," Dr. Bernard testified. She pointed to an absence of large-scale published data showing the safety and efficacy of nurse practitioners “working by themselves," adding that most nursing education programs nowadays are completely online with little in-person clinical training.
TMA shared similar patient safety concerns about allowing psychologists to prescribe and allowing pharmacists to diagnose and treat patients over the pharmacy counter.
In response to the state’s inquiry into solving Texas’ behavioral health crisis, Austin psychiatrist and past TMA Council on Legislation member Thomas Kim, MD, testified, "it would be unreasonably difficult for a non-medically educated provider – with only a few short weeks of pharmacology training – to diagnose or adequately treat [complex mental health] conditions," and "bestowing prescribing privileges to nonmedical providers is unlikely to actually solve the identified problem with access to care.”
Instead, TMA emphasized that building on the foundational systems the Texas Legislature already established is key to improving access to care. That includes:
- Investing in graduate medical education and loan repayment programs to maintain a robust physician workforce so patients have access to high-quality care across the board.
- Expanding telemedicine with physician oversight and enacting payment parity for these programs, which can expand quality medical care throughout the state, particularly behavioral health care.
- Supporting statewide broadband expansion and digital literacy for increased rural health care access
- Strengthening health plans’ network adequacy to ensure patient coverage.
Whatever the solutions, Senator Kolkhorst said they likely will be wrapped into the legislature’s base bill for state health care funding.
To stay abreast of TMA’s state advocacy efforts, check out the association’s dedicated webpage.
Amy Lynn Sorrel
Associate Vice President, Editorial Strategy & Programming
Division of Communications and Marketing
(512) 370-1384