El Paso internist Roxanne Tyroch, MD, has more than doubled the hourly rate she pays medical assistants at her practice since the onset of the COVID-19 pandemic.
“My personal strategy has been to pay high,” she told Texas Medicine. “To have high expectations but to pay high.”
Despite this steep increase in pay, Dr. Tyroch still struggles to compete for talent. She says larger practices, health systems, and immigration detention centers in town can offer even higher hourly rates, thanks in part to state and federal funding.
At the same time, Dr. Tyroch is contending with other pressures, including rising practice costs due to inflation and routine Medicare physician pay cuts, both of which threaten her practice’s viability.
“Inadequate [physician] payment in this environment is destabilizing,” she said. “We don’t have the reserves to counter payment issues.”
After nearly three years of pandemic response and amid a newly tight labor market, many medical practices are struggling with staff recruitment and retention. The main driver of practice staff turnover in 2021 was workers finding better pay and benefits elsewhere – which outpaced burnout, retirement, and other factors combined – according to a June 2022 report by the Medical Group Management Association (MGMA).
In response, practices are offering higher wages and reconsidering their divisions of labor. But these stopgap solutions may not be sustainable in the long term.
In light of these issues, the Texas Medical Association recently formed an Ad Hoc Committee on Independent Physician Practice. The 15 physician members – who hail from across Texas and practice types – are focused on developing solutions for a range of issues, including staffing shortages.
In addition, the Centers for Medicare & Medicaid Services (CMS) last year increased the clinical labor staff payment rate, which Medicare uses to calculate the cost of practice staff – including medical assistants, nurses, and imaging technicians – for a given health care service.
Although this change will lead to higher payments for some practices, it’s not a panacea. So, TMA has joined the American Medical Association and other state medical and national specialty societies in calling for wholesale reform of the Medicare physician payment system.
Without meaningful changes, practices like Dr. Tyroch’s are left to gamble, offering higher wages in hopes of attaining the staff levels needed to stay open.
But, she warned, “It’s no guarantee.”
Division of labor
Austin internist Tony Aventa, MD, and Fort Worth allergist and immunologist Sue Bailey, MD, who co-chair TMA’s Ad Hoc Committee on Independent Physician Practice, say staffing shortages are caused by myriad factors and manifest differently according to geography and practice type, making solutions elusive.
For instance, Dr. Aventa, a past president of the Travis County Medical Society, says his practice has seen strong employee loyalty overall but struggles to get enough qualified applicants when hiring for open positions.
“We do see ebbs and flows … but I do think this is a more challenging time right now,” he said.
On the other hand, Dr. Bailey, a past president of TMA and of AMA, says her practice has seen high turnover among front-desk staff. She adds that hiring office personnel has changed since the onset of the pandemic, which disrupted the labor market and left employers clamoring to adjust.
“It’s like we’re in a completely new world now,” she said. “We’re as busy as we want to be, but it gets harder and harder to keep new personnel.”
An April MGMA Stat poll found medical assistants were the most difficult position for practices to recruit (44%), followed by nurses (27%) and administrative and billing staff (18%). Practice leaders also reported that the shortage of medical assistants and other health care professionals caused more work for existing staff, exacerbating burnout and turnover rates. The resulting shortages can cause lower productivity and inconsistent hours, which in turn can affect patient volume and satisfaction.
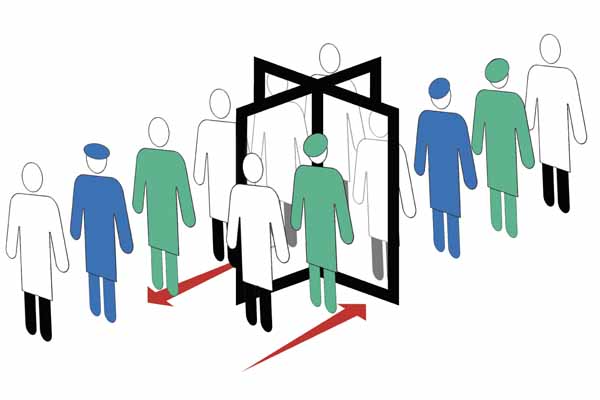
Dr. Bailey has seen this cycle play out in her practice, which has responded to staffing challenges by revisiting staff members’ job descriptions.
“One way we’ve responded … is to take a step back and take a look at everyone’s role in the office and evaluate whether the divisions of labor are appropriate and if some personnel can be more flexible with helping out with referrals or prior authorizations … than they have been in the past,” she said.
Other practices are adopting Dr. Tyroch’s strategy of “paying high.” Median hourly rates for medical assistants and nursing positions have increased by over $1 per hour in the past year and by $1.50 to over $2 per hour compared with prepandemic rates, according to the MGMA report.
Additionally, nearly half of medical groups have added or increased employee benefits in the past year, according to a May MGMA Stat poll. This represents a significant increase from June 2021, when only one in four medical groups reported adding or increasing employee benefits in the previous year.
Despite these pay bumps, physicians say staff turnover remains a concern. And Dr. Bailey worries that it is just one of several existential threats to independent practices.
“Physicians are concerned with declining [payment], the staffing issues, prior authorizations, [and] the increased cost of doing business,” she said. “Almost each one has reached a crisis level in terms of the survival of independent physician practice in Texas.”

Investing in a fix
San Antonio radiologist Zeke Silva, MD, chairs the AMA/Specialty Society Relative Value Scale Update Committee (RUC), a volunteer panel of 32 physicians and other health care professionals that makes recommendations to Medicare about physician payment. While practice expenses, including staff salaries and benefits, factor into the committee’s recommendations, the RUC has limited power to effect change without comprehensive Medicare physician payment reform, he says.
For instance, Medicare considers the RUC’s recommendations in concert with federal statutes and set formulas that govern physician payments, Dr. Silva explains. One such formula is the clinical labor staff payment rate, which Medicare increased last year for the first time in two decades, using updated wage data from the U.S. Bureau of Labor Statistics.
“If you’re getting paid more, you can pay your staff more, you can retain your staff, you can recruit staff, [and] you can maintain your practice,” he said.
While welcoming the change, Dr. Silva is quick to add that the rate increase comes at a cost. Because of federal budget neutrality requirements, which mandate that any physician pay increase or decrease be offsetting, the increase in the clinical labor staff payment rate must be counterbalanced by a decrease elsewhere.
In this case, he says the cost is borne in the payment rates related to practice supplies and equipment. So, practices with a lot of staff but not a lot of specialized equipment will see relief, while those with the inverse setup – like his own radiology practice – might see a pay cut.
“It doesn’t feel good to know that you had a win for your specialty at the expense of another specialty,” he said.
From Dr. Silva’s perspective, the solution to this problem is simple – at least in economic terms.
“You have to put more money into the system,” he said. “If you’re going to increase labor cost payments, you have to put more money into the system to accommodate that.”
But physicians know pay increases are hard to come by, even when desperately needed.
Between 2001 and 2020, Medicare physician payments decreased 22% when adjusted for inflation, where payments for other health care sectors have generally kept pace with inflation, according to AMA.
On top of this, CMS has included a 4.5% physician pay cut as part of its 2023 Medicare Physician Fee schedule, which will take effect Jan. 1 unless Congress intervenes. (See “Death by a Thousand Cuts,” November 2022 Texas Medicine, pages 42-44.)
To avoid this annual rigmarole, TMA has endorsed a set of Medicare payment policy principles developed by AMA and other medical societies that urge Congress to ensure a baseline annual pay increase that keeps up with inflation and to eliminate budget neutrality requirements.
Dr. Silva says such reform is necessary to ensure physician practices can continue to care for their Medicare patients – and to keep their doors open for everyone.
“You don’t want [patients] to feel that the physician is struggling to hire staff or to update their equipment or pay for rent,” he said. “You want them to feel well supported.”
