
In the ongoing fight to save Texas mothers from outsized rates of mortality and morbidity, medicine scored a major victory this year: the extension of Medicaid coverage for postpartum mothers to one year.
A long cry from 60 days’ coverage, the change is a culmination of a massive, long-term advocacy effort, says Sherri Onyiego, MD, a member of the Texas Medical Association’s Committee on Medicaid, CHIP, and the Uninsured.
Given the many challenges along the way – and some still ahead to fully patch together maternal coverage – the Houston family physician reminds herself to stop and appreciate the triumph.
“We’ve fought and advocated for so long, sometimes we have to take a step back and pause and just take it all in,” said Dr. Onyiego, who also chairs the Disparities Subcommittee of the Texas Department of State Health Service’s (DSHS’) Maternal Mortality and Morbidity Review Committee (MMMRC).
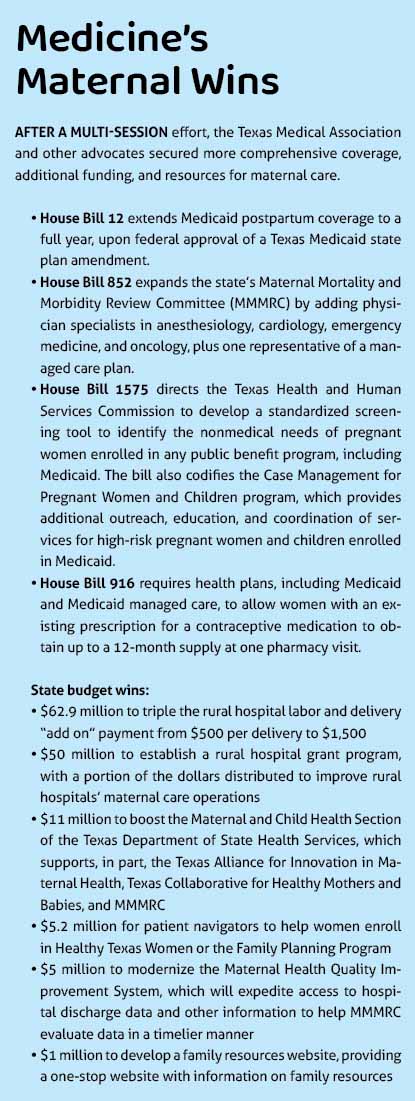
The coverage extension, achieved through House Bill 12 by Rep. Toni Rose (D-Dallas) in the 2023 regular Texas legislative session, is the centerpiece of a slate of wins medicine secured to improve maternal health. (See “Medicine’s Maternal Wins,” page 21.) Sen. Lois Kolkhorst (R-Brenham) carried the bill in the Senate.
“I don’t want to take full credit because there were so many people involved with this,” Representative Rose told Texas Medicine. “The advocates and the health care providers, health care organizations, and my colleagues. I mean, it was all of us. It just so happened that I was the one who was able to get it to the finish line, and for this I’m grateful.”
What remains is the approval of a state plan amendment to implement the law – a more straightforward process than past attempts, and one that can be turned around sooner, says Helen Kent Davis, TMA’s associate vice president of governmental affairs. She anticipates that by time of publication, the Texas Health and Human Services Commission (HHSC) will have submitted the amendment, with expectations to fully implement the legislation in early 2024.
Representative Rose says she and her office are in close contact with HHSC to ensure a smooth adoption.
The full benefits of HB 12 may be complicated by Medicaid’s ongoing eligibility redetermination process. (See “Coming Unwound,” page 26.) Beginning this fall, several TMA committees will collaborate to identify policy options Texas could consider to further improve access to women’s health care, including strengthening access to services in rural communities.
MMMRC has continually supported increased access to care during pregnancy, in the year following pregnancy, and throughout the preconception and interpregnancy periods. HB 12 only addresses part of that recommendation, but it’s a huge step forward, Dr. Onyiego says.
“[HB 12] doesn’t necessarily take away some of the issues that women still have with access to care, but it certainly goes a long way to say that they have the coverage when they need it,” Dr. Onyiego said.
A long time coming
Such success didn’t come easy.
One in three pregnancy-associated deaths in Texas occur 43 days to one year postpartum, making a full year of continuous postpartum care MMMRC’s top recommendation since the committee began issuing reports in 2018.
The same year, TMA mobilized a Maternal Health Congress, during which maternal access-to-care concerns topped the list of resultant recommendations, including providing 12 months of continuous coverage for preventive, primary, and specialty care coverage for women before, during, and after pregnancy.
The congress also called for “the implementation of hospital-based quality improvement initiatives that reduce maternal mortality and morbidity, based on best practice and standardized protocols,” in concert with the state’s rollout of the Texas Alliance for Innovation in Maternal Health (TexasAIM) program.
And over the years, versions of legislation similar to HB 12 have been filed numerous times by several lawmakers. Representative Rose personally filed the bill twice, in the 2019 and 2021 legislative sessions, before she and Senator Kolkhorst got it passed in 2023 – with the help of letters of support from more than 200 organizations, including TMA.
She specifically credits the unique bicameral, bipartisan support the bill received this year, particularly in the wake of the U.S. Supreme Court decision in Dobbs v. Jackson Women's Health Organization. The bill filed in 2019 was never assigned to committee; in 2021, a 12-month extension was negotiated to six months, and due to statutory language, the necessary waiver for that change did not clear the Centers for Medicare & Medicaid Services (CMS). This year, with support from right-to-life organizations, HB 12 received two-thirds approval by both the House and the Senate.
Continuous improvement
Though not a cure-all, HB 12 does work hand in hand with other legislative wins and state efforts to improve maternal care and related disparities.
House Bill 852 by Shawn Thierry (D-Houston), for instance, expands MMMRC by adding physician specialists in anesthesiology, cardiology, emergency medicine, and oncology, plus one representative of a managed care plan.
Because preventing maternal mortality and morbidity requires a collective approach and a range of expertise, the committee is eager to welcome new voices, Dr. Onyiego said.
“We see tremendous value in increasing the diversity of the committee. As we continue to see some of these causative underlying factors that are contributing to morbidity and mortality, we also see a greater need to have more expertise in those areas.”
For instance, having an emergency physician on board gives the committee an opportunity to learn more about emergency medical service protocols regarding pregnant patients, and a cardiologist could provide valuable care insight for hypertension and cardiovascular disease, which both greatly affect maternal health.
“I, like many others on the committee, am really excited about having those additional voices, as well as providing additional capacity to the committee as a whole,” Dr. Onyiego said.
Tackling other underlying factors in maternal morbidity and mortality, House Bill 1575 by Rep. Lacey Hull (R-Houston) directs HHSC to develop standardized screening for nonmedical needs of pregnant women enrolled in Medicaid and other state programs. Upon finding risks, Medicaid managed care organizations must provide case management services to connect a patient with medical and community services to improve birth outcomes. HB 1575 also allows community health workers and doulas to provide those case management services.
The law reinforces national and state efforts, such as the Centers for Disease Control and Prevention’s Hear Her campaign, which calls on physicians to address health disparities by identifying possible nonmedical drivers of health and avoiding stereotypes. DSHS now runs Hear Her Texas, with testimonials from patients and resources for physicians.
In its latest report, issued in 2022, MMMRC found non-Hispanic Black women are significantly more likely to experience complications relating to hemorrhage, sepsis, and preeclampsia. To determine exactly why requires further research, Dr. Onyiego says, and efforts are underway.
For its part, MMMRC’s second recommendation, after improved access to care, is to “engage Black communities and those that support them in the development of maternal and women’s health programs.” This includes bettering maternal health and safety programs and services aimed at Black women; redesigning graduate medical education to help physicians better address disparities in care; and implementing policies at hospitals and clinics designed to promote more respectful care.
“A lot of times, when Black women complain or voice a concern, they feel like they’re not being heard,” Representative Rose said. “It’s, to me, a cultural competency. Certain communities are impacted differently. It’s my hope that when women voice concerns about their bodies that [physicians] listen to them.”
MMMRC’s 2022 report also found, that in 2020, the obstetric hemorrhage hospitalization rate among non-Hispanic Black women remained high, despite hitting an overall low since 2017.
The overall drop, however, coincides with the implementation of a TexasAIM hemorrhage “bundle” in 98% of Texas birthing facilities.
These bundles are collections of evidence-based, quality-improvement best practices developed by multidisciplinary teams, including physicians. TexasAIM’s current bundles target chronic conditions both physical and mental – another key to improving maternal outcomes, beyond just coverage, because of the risks they pose in creating later complications, Dr. Onyiego says. The newest bundle, on substance use disorder, follows up on MMMRC’s recommended improvements to integrated behavioral health care access for women with mental health and substance use disorders.
“Any efforts … to support best practices in a uniform and concise way are always warranted,” she said. “For physicians to be able to provide uninterrupted care, especially if there are chronic conditions like diabetes, hypertension, asthma, things that can be controlled in a primary care setting – being able to manage those things effectively at the appropriate setting is critical.”
In light of success achieving postpartum coverage, Nancy Dickey, MD, executive director of the Texas A&M Rural and Community Health Institute, emphasized the need to stay diligent in protecting prenatal care, which she says is crucial in addressing health risks as soon as possible. Attached to prenatal care is pregnancy planning, in which medicine also gained a victory.
House Bill 916 by Rep. Claudia Ordaz Perez (D-El Paso) requires health plans, including Medicaid and Medicaid managed care, to allow women with an existing prescription for a contraceptive medication to obtain up to a 12-month supply at one pharmacy visit.
“The actual delivery care is one piece of [improving maternal care], but without great prenatal care, we won’t experience the reduction in problems that we all hope to see,” Dr. Dickey said, adding that “planned pregnancies should be high on our list anytime we talk about maternity care. If you’re not planning a pregnancy, if it’s accidental, you many times miss the early interventions: Don’t smoke, don’t drink, don’t take drugs during the formative months of your baby’s life, consumption of vitamins to reduce congenital defects. You miss all of that.”
The long haul
Meanwhile, the Medicaid continuous eligibility redetermination process all states including Texas are going through may dampen the excitement around implementation of HB 12.
About 6 million Medicaid enrollees must revalidate their Medicaid eligibility over the course of the unwinding. As of this writing, HHSC reportedly had initiated reenrollment for 2.5 million enrollees.
Although most postpartum women were not in that cohort, among the 80% of patients who have reportedly lost coverage, “I would be remiss not to think that some of those are women of childbearing age,” Dr. Onyiego said.
Moreover, Texas Medicaid’s eligibility system is struggling to timely process new applications, potentially delaying access to early prenatal care. According to HHSC data, about 24% of new applications are not processed within state-set time frames.
And many of the women declared ineligible to reenroll in Medicaid likely would qualify if HB 12 were already in place, Ms. Davis says.
Dr. Onyiego remains hopeful that other safety-net programs, such as Healthy Texas Women, can patch coverage until HB 12’s implementation is complete.
Other challenges remain, particularly as rural shortages persist, Dr. Dickey cautions. (See “The Rural Factor.”)
“Certainly Medicaid [coverage] is a substantial portion of the issue, but if you have no one in your community who provides prenatal care, it really doesn’t matter if you have a ‘ticket,’” she said. “You’ve still got to figure out, ‘Where’s the closest person that does prenatal care, and how am I going to get there?’ And if it’s 30, 40, 60 miles, the odds are good, even if you have transportation, you’re going to be less likely to get your prenatal care.”
MMMRC also continues to study additional trends, related to COVID-19, for instance – findings that will be featured in its next report due out in 2024.
As in the recent legislative session, Dr. Onyiego says future success will depend on collaboration.
“We want to make sure that the report gets in the hands of as many stakeholders [as possible] who can contribute to increasing that visibility, to help us move the needle.”
Representative Rose agrees.
“I’m going to continue working with the Maternal Mortality and Morbidity Review Committee to see what recommendations [they suggest], since they’re really the ones doing the deep dive,” she said.